Making Science Sexy: Igor Rudan's Incredible Video Series: Survival, the Story of Global Health
March 31, 2020 - Eminent Croatian scientist Igor Rudan has written some of the most authoritative and clear texts on COVID-19. Now watch him explain Survival, the Story of Global Health. Science IS sexy.
I wrote an article a couple of days ago in which I said that I was not in the habit of writing an article praising people I had never met, which is true.
And yet, here I go again... Maybe it is the cabin fever starting to show.
Croatia has many heroes at the moment, from the dedicated health workers on the corona frontline to those in power with the huge responsibility to keep Croatia safe and navigate the most unpredictable waters that the world has known in my lifetime.
And these heroes and heroines are more than rising to the task, and I think them sincerely on behalf of me and my family (and, I suspect, the rest of the country). We have already written about new Health Minister Vii Beros and the legendica that is Almenka Markotic.
And so we come to our third hero of the hour, whom I have also never met. Indeed - please don't tell him, as I am a little embarrassed to admit it - I had no idea who he was until my colleague Lauren starting translating and publishing his amazing texts about corona on TCN.
(Just like Alemka and Vili, Igor Rudan also makes the list of the current top 10 most positive people in Croatia)
And when I read the articles on corona by Igor Rudan, I felt even more embarrassed. They were the most detailed, clear and factual articles I have read since this madness began. His latest answers one of the questions that maybe people are asking, but nobody seems to know the answer to - but Igor does.
Igor Rudan Explains What Went So Wrong With COVID-19 in Italy
You can read more of Lauren's translations of Igor's corona masterpieces here.
I decided to seek him out for a TCN interview and was surprised to find that we were friends on Facebook. I have currently 3,546 FB friends, and I know about 200 of them, but many Croatians seem to like to connect with a fat Irishman living in and writing about their country, which is great.
As we were friends on FB, that made the communication easier, so I sent him a link to one of Lauren's translations and said we would be happy to do more, so that his wisdom could go beyond the confines of the svjetski jezik, hrvatski, and into English.
Not only did Igor agree, but he was happy to add his superstar name to the TCN team of writers, thereby tripling the TCN IQ in one fell swoop, insisting that the texts appear in English first on TCN, and then he hired Lauren to translate lots of his other work.
It is a marriage made in heaven, and I have not seen young Simmonds as enthused about translating since we first met 4 years ago.
An extremely funny man from our messaging exchanges, he is the person I am most looking forward to meeting after all this madness is over (as well as holding Mate Rimac to his promise to let me drive him around in his $2.75 million C2 electric wonder car - I have promised to drive slower than Richard Hammond).
And then THIS!
My wonderful wife sent me a link to a YouTube video yesterday - Igor Rudan presenting Survival, the Story of Global Health.
It is sensational! Beautifully filmed, calmly and intelligently presented by Igor himself, mostly shot in Croatia, as well as Edinburgh, where he is a Prof at the university.
We called the kids to watch it together as a family. Watching their initial lack of enthusiasm turn to fascination during the first episode was a joy.
For those of you watching reruns of NCIS and Law and Order, THIS is for you. Check out the full series below.
And the final bit of reassuring news for this article. Igor messaged us last night to apologise for a short delay in sending us an article update. He explained that he had spent most of the day advising the Croatian authorities on the response to corona.
Doesn't it make you feel just a little safer knowing that those tasked with keeping us safe are taking advice from the very best?
Igor Rudan: Cascade of Causes That Led to COVID-19 Tragedy in Italy and Other EU Countries
March the 29th, 2020 - Professor Igor Rudan is the Director of the Centre for Global Health and the WHO Collaborating Centre at the University of Edinburgh, UK; he is Editor-in-Chief of the Journal of Global Health; a Fellow of the Royal Society of Edinburgh and one of the most highly cited scientists in the world; he has published more than 500 research papers, wrote 6 books and 3 popular science best-sellers, developed a documentary series "Survival: The Story of Global Health" and won numerous awards for his research and science communication.
The perception of the COVID-19 pandemic in my homeland Croatia has been based on two main sources of information over the past three weeks. On the one hand, our Civil Protection Headquarters, as well as all of the experts and scientists to whom media space has been provided, called for caution, but without any panic. They emphasised that this was not a cataclysm, but an epidemic involving a serious respiratory infectious disease. The cause of this disease is the new coronavirus, for which we don’t have a vaccine. Therefore, it can be expected that the disease will be very dangerous for the elderly and to those who are already ill. So, it was an unknown danger worthy of caution, but our epidemiologists remained calm. They knew that they would be able to estimate the epidemic's development using figures, and then control the situation with anti-epidemic measures, and through several lines of defense.
On the other hand, we also followed the events in Italy. From there, day after day, apocalyptic news came, with incredibly large numbers of infected and dead people. Daily reports from Italy seemed completely incompatible with what the experts and scientists in Croatia were saying. Some have concluded that a scenario similar to that in Italy, if not worse, is inevitable for Croatia. The population was in a very confusing situation.
In this text, I will try to penetrate the very core of the "infodemia" that has been present in the media across many European countries, as well as on social networks, over the past three weeks. I will explain how that disturbing situation arose and offer a scientific explanation for it. This seems important to me at this point, because the Italian tragedy with the COVID-19 epidemic has, unfortunately, hindered the credible and scientifically based communication of the epidemiological profession to the population of Croatia.
In my article "20 Key Questions and Answers on Coronavirus" posted on the 9th of March, 2020 on Index.hr, in answer to question number 18, "With the effectiveness of quarantine in China, can we draw some lessons from this pandemic?", I stated:
"If the virus continues to spread throughout 2020, it will demonstrate in a very cruel way how well the public health systems of individual countries are functioning… These will be very important lessons in preparation for a future pandemic, which could be even more dangerous.’’
We’re now slowly entering a phase where many countries have been exposed to the pandemic for long enough. Thanks to this, we can make some first estimates of their results. From these days up until the end of the pandemic, we’ll see that COVID-19 will divide the world into countries that have relied on epidemiology and followed the maths and the logic of the epidemic, as well as those in which this isn’t the case, and many sadly, probably quite unnecessarily - will suffer.
An epidemic is a serious threat to entire nations, during which residents' interest in other topics may vanish quite rapidly. We could see that happening quite clearly in the past several weeks. The task of epidemiologists is to constantly have tables in front of them with a large number of epidemic parameters, reliable field figures and formulas to monitor the epidemic's development, and to know the ‘’laws’’ of epidemics, in order to organise the implementation of anti-epidemic measures in a timely manner and thus protect the population.
Now, let's look at the countries that we can already point out as being successful in their response to this new challenge. First and foremost, there’s China. It has completely suppressed the huge epidemic in Wuhan, which spread to all thirty of its provinces. In doing so, it relied on the advice of its epidemiologic legend, 83-year-old Zhong Nanshan. Twenty years ago, Nanshan gained authority by suppressing SARS. Although surprised by the epidemic, they managed to suppress COVID-19 throughout China through expert and determined measures. They did so over just seven weeks, with the death toll eventually coming to a halt at less than 5,000. By comparison, it would be as if the number of deaths in Croatia as a result of this epidemic was kept at around 14 in total.
Furthermore, if at some point you find yourself caught up in the uncertainty surrounding the danger of COVID-19, you will easily be able to find out the truth if you look at the state of things in Singapore. Despite intensive exchanges of people and goods with China since the outbreak of the epidemic, Singapore has a total of 732 infected people as I am writing this article, with two dead and 17 more in intensive care. This city-state has the ambition to be the best in the world in all measurable parameters. From this, it must be concluded that the developments in Singapore are a likely reflection of the real danger of COVID-19. However, this is true of countries that base their regulation on knowledge, technology, good organisation and general responsibility. The situation in Singapore, therefore, is an indicator of the effects of the virus on the population, to the extent that it is truly unavoidable.
Any deviation towards something worse than the Singaporean results will be less and less of a consequence of the danger of the virus itself, and increasingly attributable to human omissions. In doing so, human errors that can lead to the unnecessary spread of the infection are: (1) the epidemiologists' omission to properly understand the epidemic parameters; (2) decision-makers' reluctance to make decisions based on the recommendations of epidemiologists; and (3) the irresponsible behaviour of the population in complying with government instructions.
To confirm the statements about Singapore, let's look at the current situation in other countries that rely on knowledge and expertise and have good organisation. They were also the most common destinations for the spread of the epidemic from China in the first wave: Hong Kong, Japan, South Korea, the United Arab Emirates and Qatar. There were only 519 infected people in Hong Kong at the time of writing this article, with 4 deaths and 5 more people in a serious condition; in Japan 1,499 were infected, 49 were dead and 56 were in a serious condition; in South Korea, which had a severe epidemic behind its first line of defense, 9,478 were infected, 144 died and 59 were seriously ill; in the United Arab Emirates, 405 were infected, 2 died and 2 were seriously ill; and in Qatar, 562 were infected, 6 were seriously ill, and still no one had died from COVID-19.
Fortunately, Croatia is now up there with all of these countries, with 657 infected, 5 dead and 14 more seriously ill. As you can see pretty clearly from all of these figures, in countries that rely on knowledge and the profession and properly applied anti-epidemic measures, COVID-19 is a disease that should not endanger more than 1 percent of all infected people. This conclusion can be reached by considering that the information on the "https://www.worldometers.info/coronavirus" page is based on positive tests, and not on everyone who is actually infected.
What, then, is happening in Italy, as well as in Spain, but to a good extent also in France, Switzerland, Belgium, Austria, Denmark and Portugal? I did not include Germany, Sweden, the Netherlands, the United Kingdom and the United States in this group of countries for now. This is because at least for some time during the epidemic, they have clung to the idea of intentionally letting the epidemic develop and infect at least part of the population, so I will refer to their strategies and their results in one of my following texts.
Given all of the previous examples of a successful epidemiological response, and what is now practically the coexistence of people with the new coronavirus in Asia's most developed countries, how is it possible for Italy to have nearly 85,000 infected people and over 9,000 deaths at the time of this article? How is it possible that Spain has 72,000 infected people and more than 5,600 deaths, and France has almost 33,000 infected people and 2,000 deaths? Or that even Switzerland, which everyone would expect to see among the most successful countries in any of these world rankings, could already have 13,250 infected people and 240 deaths, with 203 more critically ill people? The causes of all of this are, however, becoming increasingly clear to science.
First of all, there was probably a premature relaxation around the real danger of COVID-19 in Europe. The epidemic development by the end of February was already quite similar to the one seen previously with SARS and MERS. Even then, the primary focal point was suppressed, and in more than 25 countries, the virus was then stopped at the front lines of defense. By the end of February 2020, it was already clear in the case of COVID-19 that it would be successfully suppressed in its primary focal point - Wuhan. It was also already stopped at the front lines of defense in another thirty Chinese provinces and surrounding countries in Asia. Then, on February the 28th, the first estimates of death rates were published, saying that it was a disease with a death rate significantly lower than that of SARS and MERS. At that time, it was reasonable to expect that the epidemic could soon be
stopped. As a result, the World Health Organisation delayed the declaration of a pandemic until March the 11th, and the world stock markets increased by about 10 percent from February the 27th to March the 3rd. But for any unknown virus, premature relaxation is very dangerous, as will be shown later with COVID-19.
Secondly, several investigative journalists reported that it may be possible that the phenomenon of the mass immigration of Chinese workers to northern Italy may have contributed to the early introduction and spread of the virus in Europe. Tens of thousands of Chinese migrants work in the Italian textile industry, producing fashion items, leather bags and shoes with the brand "Made in Italy". Partly as a result of this development, direct flights between Wuhan and Italy were introduced. Some estimates say that Italy has allowed up to 100,000 Chinese workers, initially from Wenzhou, but later also likely from Wuhan and other cities neighbouring Shanghai, to work in those factories. Some of them may have been there illegally and worked in conditions where they were cramped together, which would help the virus to spread easily. Reporter D. T. Max wrote about this phenomenon in the New Yorker magazine back in April 2018. After their return from the Chinese New Year celebrations in mid-February, the Italian authorities rigorously checked these workers on their "first line of defense" at the airports. But rumours began spreading that some had begun to enter Italy but were bypassing Italian airports. Instead, they were going through other airports in the EU where controls weren’t as tight. So, the COVID-19 epidemic was likely triggered behind the back of the Italian "first line of defense", which remained unrecognised in the first few weeks.
Third, many infected people from northern Italy spent their weekends at European ski resorts. Although we don’t know if the arrival of the warmer weather will stop the transmission of coronavirus, what we can assume is that the cold helped it to spread. That is why European ski resorts became real nurseries of coronavirus in late February and in early March. In this way, more infected people emerged behind the front lines of defense in France, Switzerland, Belgium, Austria, Denmark, Spain and Portugal. Their first lines of epidemiological defense focused on air transport from Asia, not on their own skiing ‘’returnees’’, where indeed no one would expect a large number of Chinese people from Wuhan to be.
Fourth, although Spain may not have had as many skiers as other European countries in this cluster, the virus may have been introduced to them through a "biological bomb". On February 19th, a Champions League football match was held between Atalanta and Valencia. Atalanta is a team from a small city of Bergamo, Italy, which has 120,000 inhabitants. This was possibly the biggest game in Atalanta's history, as it progressed through group stages to the last 16 in the European Champions League. The local stadium was not large enough for everyone who wanted to attend the game, so it was moved to a large San Siro stadium in Milan.
The official attendance was 45,792, meaning that a third of Bergamo’s population, with around 30 busses, travelled from Bergamo to Milan and then wandered the streets of Milan before the game. Unfortunately for Spain, nearly 2,500 Valencia fans also traveled to the match. As Atalanta scored four goals, a third of Bergamo's population was hugging and kissing in the cold weather four times and spent the day closely together. This is likely why it became the worst-hit region of Italy by some distance. Unfortunately, at least a third of the Valencia football squad also got infected with a virus and later played Alaves in the Spanish league, where more players of that team got infected. This football game has certainly contributed to the virus making its way to Spain.
Fifth, it’s very important for the early development of the epidemiological situation in each country to look at which subset of the population the virus has spread among. Northern Italy has a very large number of very old people. In the early stages of the epidemic, the virus began to spread in hospitals and retirement homes. They didn’t have nearly enough capacities to assist in the severe cases. Among already sick, elderly and immunocompromised people, the virus spread more easily and faster and had a significantly higher death rate. In some other countries, such as Germany, most of the patients in the early stages were between the ages of 20 and 50, and were returning from skiing trips or were business people. Therefore, such countries have a significantly lower death rate among those first infected.
Sixth, and what the most important thing needed to understand the current situation in Italy is, must have been either the omission of Italian epidemiologists to monitor the mathematical parameters of the epidemic, or perhaps their lack of clear communication of the dangers to those in power in northern Italy, or the indecisiveness of those in power to adopt isolation measures for the population. It is difficult at this time to know which of these three causes is the most important, and a combination of all of them is entirely possible. However, I will explain the nature of the omission, as it largely explains the terrible figures on infections and deaths that are being reported from Italy on a daily basis.
To understand the story of this tragedy in Italy, we must first return to Wuhan. When the epidemic broke out, the Chinese first had to isolate the virus. Then, they needed to read its genetic code and develop a diagnostic test. It all took time, as the epidemic spread rapidly throughout the city. When they began testing for coronavirus, between January the 18th and the 20th, they had double-digit numbers of infected people. Those numbers apparently stagnated, so the epidemiologists didn't know what that might mean. But on the 21st of January, the number of newly infected people jumped to more than 100. On the 22nd of January, it jumped to more than 200. This was a clear signal to Chinese epidemiologists that an exponential increase in the number of infected people was occurring. At that time, they had nothing further to wait for, or to think about. If the virus breaks through the first line of defense - and the Chinese didn’t even have any, since the epidemic started there - then a quarantine measure needs to be triggered. This prevents the virus from spreading further and creating a large number of infected people through exponential growth.
After such a sudden declaration of quarantine in Wuhan, the huge epidemic wave of the Chinese had actually just begun to show. Everyone who was already infected began to develop the disease in the next few days. The maximum daily number of new infected cases was reached on the 5th of February. On that day alone, as many as 3,750 new patients were registered in Wuhan. Remember, this means that the jump from about 125 to about 250 registered newly infected people signals to epidemiologists that we should expect an epidemic surge in 14 days, with as many as 3,750 newly infected people in one single day.
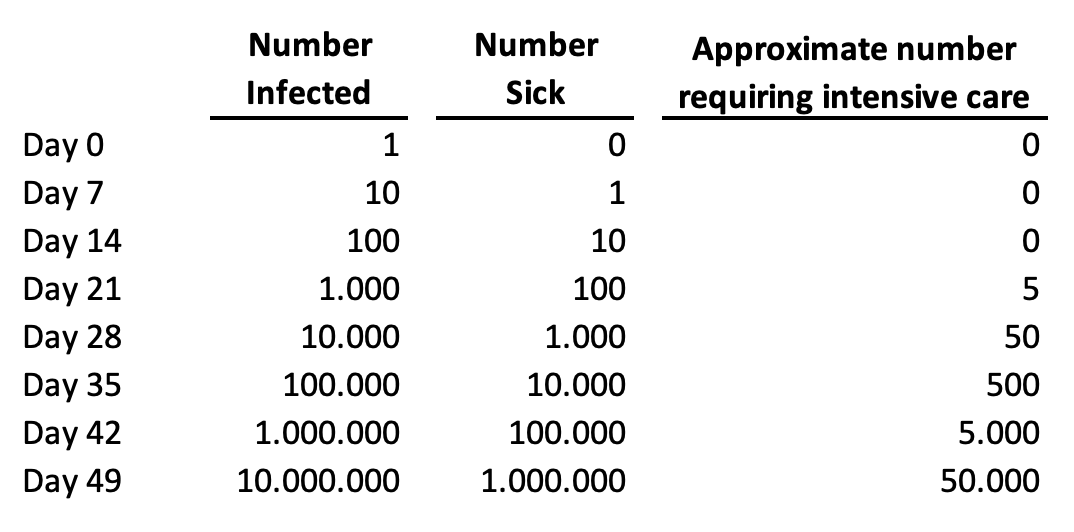
Let's now explain this "time delay" between people getting infected with the virus and the health system being able to detect all those infected people based on their symptoms. The new coronavirus kills primarily because it spreads incredibly quickly among humans. As a result, it creates a gigantic number of infected and sick people in a very short time period. Among those who are sick, about 5 percent will require hospital care. If all of them could receive optimal care, we'd be able to save nearly everyone. But if they all get very sick at the same time, we can't offer them adequate care and nearly all of the critical cases will die. This is the primary way in which this virus kills so many people. It is illustrated in a very simple way in this table, based on day-to-day growth in a number of cases by 26 percent, which was a very realistic scenario for most EU countries:
TABLE ONE: The dynamics of the epidemics of COVID-19 in any given country, based on a realistic scenario of about 26 percent of day-to-day growth of the number of cases:
With this in mind, let's now look at the Italian reaction to their own epidemic. In the early stages of infection spreading in a country, one or two infected persons are usually detected daily. Personally, I advised the Croatian authorities and public to start seriously thinking about social exclusion measures when they noticed the first notable shift from the first 10 confirmed infections towards the first 20 infected people.
On March the 12th, I posted a Facebook status entitled "Contrast is the mother of clarity", which was viewed and shared by many thousands of my fellow Croatians who have been following my popular science series on the pandemic - "The Quarantine of Wuhan". This status has also been shared by many online and printed newspapers and media, including radio stations. In that status, I suggested that Croatia should consider a large quarantine because we had already jumped from 14 to 19 infected people the day before, but to also weigh this against the economic implications and their expected effect on health. The very next day, a decision was made to close the schools.
That meant that, up to that point, Croatia completed two of the most important tasks in this pandemic. The first task was to hold its first line of defense. This was being achieved through the identification of infected cases imported from other countries and their isolation, and that of all of their contacts. Croatia completed this first task better than the other EU countries did, based on an average percentage increase of cases between the 3rd of March and the 17th of March. Then, from March the 13th, Croatia also began to introduce social exclusion measures at the right time, thus successfully carrying out the second key task in controlling its own epidemic. Many credits go to its epidemiologists who work at the Croatian Institute for Public Health.
But, what went wrong with these two measures in Italy? On the 21st of February, their number of confirmed infected cases jumped from 3 to 20. As Italy is a more populous country than Croatia, it might have still been too hasty to send all of Lombardy into quarantine based on this. But on the 22nd of February, the jump was from 20 to 62 cases, and they already needed to think very seriously about it. A couple of days later, on the 24th of February, they reached a situation very similar to that in Wuhan as the number of confirmed infections jumped from 155 to 229. This was particularly worrying because they didn't seem to be performing many tests proactively at that time, either.
That "jump" from 155 to 229, in combination with the Wuhan experience, should have suggested that they would have at least 50,000 infected people under the predicted curve of the epidemic wave and they were just seeing its early beginning. And that many infected people would mean that about 2,500 affected would require intensive care units. At the time, Lombardy had only about 500 such units in government/state facilities and another 150 in private healthcare facilities. As early as 24th of February it was clear that there would be many deaths in Lombardy weeks later. With epidemics, everything goes awry because the infected get sick a week later, and some of the patients then die ten to twenty days later, so the time delay is always an important factor that needs to be taken into account.
However, even then, the Italians didn’t declare a quarantine. They didn’t do so on the 29th of February, either, when the total number of infected people rose from 888 to 1128. Those figures implied that in mere days they would be having about 15,000 newly infected people each day. Moreover, they didn’t declare quarantine on the 4th of March, either, when the number of infected people exceeded 3,000, and when the world stock exchanges started to fall again. It had then become clear to most epidemiologists who have been advising global investors that an unexpected and major tragedy was about to unravel in Italy and this was now inevitable. At that point, Italy already had at least 30,000 infected people spreading the infection. The quarantine was declared for Lombardy on the 8th of March. The day before, the number of cases had already risen, and exponentially so, to as many as 5,883.
To appreciate the problem with epidemic spread in the population behind the first line of defense, this is similar to borrowing 1,000 Euros from someone on the 29th of February with an interest rate of 26% each day, meaning an interest rate of 26% on top of that the next day, and so on. Furthermore, there didn’t seem to be enough clear and decisive communication with the public. The news of the quarantine for Lombardy was, in fact, leaked to the media before it was officially announced. This led to a quick ‘’escape’’ of many students to the south of the country, to their homes, carrying the contagion with them. As a result, a day later all of Italy had to be quarantined.
In an already difficult situation, where every new day of delay meant another thousand or more people dying, as we can all notice these days, there were numerous media reports warning that the population may not have taken those measures as seriously as the Chinese when they introduced orders to their population in Wuhan. Any indiscipline under such grave circumstances could have allowed the virus to take yet another step quite easily. With each new step, another 26% of interest was added to everything before that, and then 26% on everything on everything before that again. That is the power of exponential growth, characteristic of free spread of the virus in the population.
Many Italians and then Spaniards, as well as residents of several other wealthy countries in Europe, had their lives cut short by their lack of recognition of the dangers of exponential function during the spread of the epidemic. Delaying quarantine for a week made the epidemic ten times worse than it should have been. Delaying it for two weeks made it a hundred times worse. And after two weeks of it being finally proclaimed, all those who may have not taken the orders seriously enough would have made the epidemic several hundred times worse. This means that, in Italy, and possibly in Spain, too, we are now observing the COVID-19 epidemic that is more than a hundred times worse than it should have been in a country that was much better prepared for the response, such as Singapore, Taiwan, Hong Kong or the United Arab Emirates.
To appreciate what is happening in Italy, it is enough to think of this sentence alone: at least 100 times fewer people would die each day if quarantine had been declared 2 weeks earlier and had the population stuck to the recommendations. During those fourteen days between 23rd of February and 7th of March, they unnecessarily allowed the virus to spread freely and infect a huge number of people - maybe even up to a million, or perhaps more, it is very difficult to know at this point. This would mean tens of thousands of people in need of intensive care, with about ten times fewer units available nationwide. About half of those who fall seriously ill will not survive without necessary support. At this point, whenever we hear that 1,000 people died in Italy in one day, we should know that the casualties would only add up to 10 had the quarantine been declared just a couple of weeks earlier. I appreciate that it seems implausible that the delay of a political decision like the introduction of quarantine by just two weeks may mean the difference between 100 deaths and 10,000 deaths in the 21st century, but I’m afraid that is unfortunately the reality of the exponential growth of the number of infected during an epidemic.
What does this mean for the public in countries like Croatia, who were confused and in awe of the events in Italy? They should know that they didn’t observe what the COVID-19 epidemic should actually look like in a country where the epidemiological service and its communication with those in power works well, as it does in Singapore, Taiwan or South Korea. In Italy, we have unfortunately noticed the consequence of an omission of epidemiologists and those in power to protect the people from the epidemic. Such a development was not predictable at all. The biggest surprise of this pandemic to date is undoubtedly the lack of response by the Italian authorities to the apparent spread of the pandemic at an exponential rate for two weeks, leading to a very large numbers of infected people in a very short time. But, it is even more surprising that, although the Italian example exposed the lack of capacity of their healthcare system to provide care to all those in need, a similar scenario is now happening in several other European countries in this group, that I initially singled out.
How and why could something like this happen in Italy and then in other countries in the European Union (EU)? I will try to offer at least some hypotheses. First, EU countries have been living in prosperity for decades, focused mainly on their economies. Aside from the economic questions, they haven’t had any challenges that they’ve had to answer to swiftly and decisively, that would measure up to this one. Back in the 1960s, vaccines were introduced against most major infectious diseases, especially childhood ones. Malaria is no longer present in Europe and tuberculosis has been treated similarly for decades. The challenge of HIV/AIDS in the 1980s is now being successfully controlled with antiretroviral drugs. Liver inflammation is treated mainly by clinicians. The impact of influenza is controlled through vaccination while rare zoonoses are resolved with immunoprophylaxis. Even sexually transmitted infectious diseases (STDs) are no longer as significant since the vaccine for Human Papillomavirus (HPV) was licensed.
The last real epidemic that concerned Europe was the Hong Kong flu, which occurred back in 1968 and 1969. The broad field of biomedicine offers such a wide range of exciting career paths to all those students who study it these days, but the epidemiology of infectious diseases is certainly not one of them, at least it has not been in Europe for a very long time. It has probably begun to seem as an archaic medical profession to the large majority of students and young medical doctors. It seemed to belong to the past for the European continent, which made it one of the least attractive things to specialize in. Even the rare epidemiologists who specialized in infectious diseases have begun retraining for chronic non-communicable diseases, due to the aging of Europe's population, which is particularly the case in Italy and Spain. It seems that at least some EU countries may have fallen victims to their own, decades-long success in the fight against infectious diseases. They faced this unexpected pandemics with few experts that could have had any experience in these events. Asian countries, as well as Canada, have had enough recent experience with SARS and MERS, but some European countries seem to have forgotten how to fight infectious diseases. If it were not for the legacy of the great Croatian epidemiologist and social medicine expert and global public health pioneer Andrija Štampar, and the relatively recent war in Croatia, it is difficult to say whether or not Croatia would be as ready as it has proven to be.
Another thing that likely undermined the Italians response was that no one before Italy, in fact, could have seen how fast COVID-19 was spreading freely among the population. The absolute greatest danger of COVID-19 is its accelerated, exponential spread when it breaks through the first line of defense. However, no-one had the opportunity to study this thoroughly before it reached Italy. Previously, only the Chinese in Wuhan and the Iranians had experienced the free spread of the infection. After five days of monitoring the number of infected, the Chinese had to quarantine Wuhan, and further 15 cities a day later, in order to contain the virus. They did not know how many infected people were outside of their hospitals. For Iran, however, no one knew exactly what was happening there, as that country is significantly isolated internationally due to political reasons. The Koreans, however, had a limited local epidemic but not an uncontrolled free spread - they caught the virus using their first line of defense.
That’s how the Italians ended up becoming the first country in the highly developed world to monitor their epidemic spreading uncontrollably among the population. The only estimate of the rate of spread of the virus to date has been in the scientific work of Qun Li et al. from the 29th of January, published in the New England Journal of Medicine. However, it was difficult for them to subsequently determine R0 parameter on the first 425 patients in Wuhan. Their estimate of the R0 for COVID-19 was 2.2, but with a very wide confidence interval - from 1.4 to 3.9. It's a bit of tough luck again that they calculated the lower bound of the confidence interval to be 1.4 exactly, because this figure is well known to all epidemiologists. It's the rate of the spread of seasonal flu in the community. It should come as no surprise that many epidemiologists would guess that, with more data, R0 for COVID-19 would start converging more towards 1.4. Unfortunately, the more recent data suggests that R0 is more likely to lean towards 3.9, implying an incredibly fast spread. Thus, the greatest danger of COVID-19 remained unrecognised in Italy until the 8th of March quarantine measures. At least 100 times fewer people would be dying in Italy these days had they declared a quarantine for Lombardy two weeks earlier than they did.
Just a few days ago, the JAMA journal published another extremely useful piece of scholarly work, authored by Odner et al. Their contribution finally provided answers to three great unknowns about COVID-19. Many myths about the situation in Italy have been present in the media since the very outbreak of the epidemic, but thanks to just one simple table, today we can finally dispel them all.
The first is the question that has plagued us all for a long time - how dangerous is COVID-19 for younger age groups? It is clear that the media will tend to single out individual cases of death in younger people, as they are of most public interest. However, it’s interesting that until recently, we didn’t have decent data on this. The first reason was that the Chinese Centre for Disease Control reported all deaths in Chinese epidemic using age group structure that contained a very large age group of "30-79 years". It only separated children up to 10 years, then adolescents up to 20 years, then 20-29 year-olds, then this huge group, and then those who were 80 years of age or older. That’s why the work of Odner and colleagues is commendable, as they made an effort to divide this large group into 10-year age groups. This finally allowed a comparison between the first 1,023 deaths in Wuhan (up to the 11th of February) with the first 1,625 deaths in Italy (up to the 17th of March). The comparison is shown in the Table 2 below. It gives us some very important insights.
Firstly, in Italy, more than half of the deaths initially were among people who were older than 80 years of age, and a total of 88% of the deaths occurred among the persons over 70 years of age. So, contrary to the impression that individual media reports can easily make, COVID-19 is a very dangerous disease mainly for the old people. Moreover, a study by A. and G. Remuzzi in the March 2020 issue of Lancet showed that, among 827 deaths in Italy, the vast majority of those people were already severely ill with underlying diseases, such as cardiovascular disease, diabetes and malignancies. This is what epidemiologists expected, because a more severe flu would have had a similar effect if there was no vaccine available. However, I doubt that the general public have the proper insight into this issue from many media reports.
Secondly, it was suggested in the media across Europe that the virus in Italy may have mutated and become much more dangerous. However, Table 2 shows that death rates by the age of 70 are practically the same in China and Italy. Then, although the case fatality rate appears to be about 50% greater in Italy than in China for the age group 70-79, this does not suggest that the virus may have mutated. It is known that in Wuhan, many of the affected with a severe clinical presentation of COVID-19 could rely on the two newly built hospitals and respiratory aids that the military had brought in from other parts of China. They also had medical teams coming in from other provinces. In Italy, however, there were not enough respirators for this age group, and there weren’t enough doctors either, as many of them themselves became infected. For those two reasons I would, in fact, expect even a larger difference between Italy and China than the one we’re seeing, so I would not attribute this observed difference to the impact of the virus itself. And finally, the reported difference in case-fatality rates for the oldest age group should also not be attributed to the virus. It is more likely a consequence of the fact that Italians of Lombardy live, on average, longer than the Chinese of Wuhan. Therefore, there are significantly more people in the oldest age group in Italy, ranging to much higher ages, so the two oldest groups are not really comparable. The average age of the Italians in the age group "80 years or older" is significantly greater than the average age of the oldest Chinese age group. Therefore, the table shows practically equal death rates across all age groups, on sufficiently large samples, meaning that the virus didn’t mutate in Italy from the virus we see from Wuhan, at least not until the 17th of March, 2020.
TABLE TWO: Adapted from: Graziano Onder et al. COVID-19 Case-Fatality Rate and Characteristics of Patients Dying in Italy. JAMA, March 2020.

Thirdly, and perhaps most importantly - this chart has now made it quite clear that COVID-19 does not, in fact, kill people under the age of 50 unless they have some sort of underlying disease, or some unknown "Achilles heel" in their immune system that makes them particularly susceptible to the virus. There are such cases with every infectious disease. They are also present during the flu epidemics, but they are extremely rare. This suddenly gives us another possible quarantine strategy, where children and those under 50 years of age could first emerge if they don’t have any underlying illnesses. Here, after this table, it already seems like we are beginning to have an increasing number of options to get out of quarantines and learn to live with this virus until the vaccine becomes available. However, at least a few more studies need to be carried out to confirm that this age group can be substantially protected, to provide reassurance that the virus is not becoming more dangerous for those younger than 50 years old, too.
There is another strangeness to the situation in Italy that will not be intuitive to the general public. The actual number of deaths attributable to COVID-19 in Italy will not be possible to estimate for several months after the epidemic finally ends. Namely, at present, due to the sole focus on the epidemic, all of the cases of death of very old people who have been diagnosed using a throat swab have been attributed to COVID-19. However, once the epidemic is over, it will be necessary to compare the deaths in individual areas of Italy with the average for the same months in the previous few years. It could be shown that a part of the already ill would have died in the same month or year even without being infected with the new coronavirus, and that COVID-19 accelerated this inevitability by a few weeks or months. In this case, the so-called "reclassification" of causes of death will need to be carried out. The deaths observed during the epidemic in Italy will be attributed to underlying diseases in accordance with expected levels, and only those above expected levels will be attributed to COVID-19. This could ultimately reduce the number of Italians who actually died of coronavirus and otherwise would not have passed away that year.
This article provides an explanation from the epidemiologist's point of view for everything that has happened so far in Italy, and then followed in Spain and other European countries where COVID-19 has expanded through ski resorts and football games. Simply, a combination of an early relaxation, a possible inexperience in the management of infectious diseases, a systemic lack of expertise in the field, a possible evasion of immigration regulations, and a series of further misfortunes and human omissions have all led to the late withdrawal of Lombardy into quarantine. This allowed for a large number of people to be infected and severe illnesses led to death due to respiratory failure. In 88% of cases, people over 70 years of age died, who, in the vast majority of cases, had underlying illnesses already. But this is an analysis based on the first 1,625 deaths in Italy, and by the time of this writing, there are now more than 10,000 dead. Given the size of the population, this would correspond to 670 deceased in Croatia, which means that in Italy it is more than 100 times worse than it is in our country. This difference may be attributable almost entirely to a two-week quarantine delay.
These days, the people of Italy, Spain and other European countries are suffering large losses because of the problem that the human brain simply cannot intuitively grasp the power of exponential growth, nor that two weeks of delay could make the difference between 100 and 10,000 deaths. Any physics enthusiasts will know that the great Albert Einstein once warned us about this - he said that interest rates, which lead to exponential growth, are "arguably the most powerful force in the universe," to which no black hole is equal.
This text was written by Igor Rudan and translated by Lauren Simmonds
For rolling information and updates in English on coronavirus in Croatia, as well as other lengthy articles written by Croatian epidemiologist Igor Rudan, follow our dedicated section.
Igor Rudan: How Can We Move from Defence to Attack in Coronavirus Fight?
Why does the director of the World Health Organisation keep repeating: "test, test, test"? How are the conditions for quarantine created, how might coexistence with coronavirus look, and how can the virus be attacked?
As Igor Rudan/Vecernji list writes on the 26th of March, 2020, Croatia has become a major quarantine - temporarily. This prevents the new coronavirus from spreading too quickly. As a result, the number of serious COVID-19 cases in our country shouldn’t increase too rapidly. This will enable our healthcare system to help anyone who develops a more severe form of the illness. Our healthcare professionals will save many lives in the coming weeks. If we all adhere to the quarantine provisions, our health care system will continue to be able to help those with other illnesses in need of intensive care. By staying in our own homes, we’re all now protecting our health care system from overloading, which could otherwise occur under the pressure of too many coronavirus patients.
After all of us found ourselves in such an unusual situation, many people have been asking me questions over recent days. The most common of these are: "What will happen next?"; "How long will this last?"; "Why didn't we test a lot more and avoid quarantine, like some Asian countries did?" Many people are also wondering if we really have to threaten the economy this way in order to, as they say, "extend the lives of those among us who are already the oldest and the most unwell?"
It isn’t even clear to many why societies have created a climate that stops people's "right to die from COVID-19"? By comparison, about eight million people worldwide die directly from smoking annually. Nearly one million of those deaths are of non-smokers, who smoke their household members’ cigarette smoke. Why aren't the deaths of all these hapless "passive smokers" tracked in the same way? Furthermore, more than one million people die each year in road accidents. All drivers are exposed to it, but not everyone survives it, nor are they always guilty of it. Why is exposure to coronavirus different from driving exposure? Finally, about one million people die of AIDS a year. However, even with the total of ten million deaths per year, nobody is stopping people from smoking, driving cars, or having sex among their population. And now, because of COVID-19, we're all in our houses at once. We are also at risk from viruses and economic catastrophe, and obviously from earthquakes.
What’s going on here, then? Why are half a million people who end up dead from the flu every year completely uninteresting to the general public, but any deaths from COVID-19 are interesting to the point that country after country in the developed west sees this as economic suicide? Or, why aren’t the six million deaths of poor children worldwide interesting to the public? It seems that it would be even more reasonable to save the victims of all the aforementioned diseases than the predominantly retired, elderly and sick people around the world who are now at risk of being infected with COVID-19.
These are not simple questions at all and I'm not sure I have clear answers to them. I’m pleased, however, that the first clear plans, scientifically based ones, are finally coming out, on how to get out of this situation relatively quickly with minimal human casualties and avoiding the complete collapse of the economy.
The first step of all these plans is always to quickly and decisively close the pathways of further spread off to the virus. This avoids creating the situation of having too many infected people too quickly. The health system is then protected from complete collapse and many human lives will be saved. After that, there is a very wide range of further options. The author Tomas Pueyo recently outlined the currently most sensible coronavirus strategy and called it "The Hammer and the Dance." I expect that over the next few weeks, the governments of many developed countries will resort to some variant of this solution, because it’s reasonable. It protects people's lives and it protects the health system, but it also protects the economy. The ‘’hammer’’ is an intensive and not too long of a quarantine that reverses the flow of the epidemic and reduces the number of infected people. The ‘’dance" is then our coexistence with the virus, much like the escalation of Muhammad Ali-style strikes, where we must never again allow it to spread quickly to a large number of people.
Therefore, once this unusual situation is over, the assessment of each country's performance in dealing with the coronavirus crisis will be based on the following five questions:
1. How long and effectively did the "first line of defense" manage to prevent the free spread of coronavirus among the population? In the case of Croatia, we were practically the best in Europe.
2. When the virus broke through the "first line of defense" and began to expand exponentially throughout the population, how quickly and decisively was a strict quarantine measure activated? In the case of Croatia, the activation measures started at the right time, with the plan being not to have the number of infected people reach more than a few thousand and for the number of serious cases to reach only a few hundred. Were it not for the earthquakes and the fleeing of many from Zagreb down to the south, these figures would probably have been reached, but we’ll see in a few days just where the number of infected people will peak.
3. How closely did the population adhere to quarantine? We’re now dependent on the discipline of all of us, so that the problems that the Italians and the Spaniards now have because of their indiscipline don’t happen to us. So stay, if you can, inside your houses.
4. How fast and active was the state in mobilising its capacities and human resources, as well as creative and innovative solutions, to develop a concrete plan for quarantining and coexistence with coronavirus as quickly as possible? This is the next urgent task for Croatia. This will include the empowerment of technological capabilities and human resources for virus testing, innovative ideas on social removal measures, effective virus control measures, the use of technologies to understand human contacts and the spread of viruses, and other things.
5. How effectively, after quarantine, has the state allowed its inhabitants to move into a relatively normal life situation and preserve their economy from collapse, with permanent control over the spread of the virus? This is our fifth task, but it isn’t one that is unsolvable either.
How are we going to achieve this over the next month, and how can we continue after that? I will try to explain this with this simple story, which will explain our current situation to you, and the options at our disposal.
Let's first imagine the whole of Croatia as a group of one hundred people. Working on their computers, the group works a night shift at an office on the ground floor near Maksimir forest.
You can enter this ground floor through a rather long corridor. In Maksimir forest, as we know, there is a zoo. It is also said that a vampire wanders through the forest at night. Due to the proximity of wild animals and these rumours of a vampire, these one hundred office employees created a round ‘’net’’ made of very tough rope. They also tied one hundred bricks around the round edge of that net.
One night, a tiger escaped from the zoo. We heard about it on the radio and hoped it wouldn't come right to us, but we still pulled that net out of the closet. A moment later, the tiger walked right into our office. We threw the net at it and then each one of us firmly gripped those bricks on its edge and pressed the net down against the floor. As strong as it was, the tiger was now pressed down by the net thanks to the joint action of all of us one hundred people.
The tiger can't really do us any harm as long as each of us presses their own brick firmly against the floor. This is our current situation with coronavirus, this is quarantine.
However, all the tiger wants to do is take away just one of us and eat that person somewhere in the woods. He would leave everyone else alone and return again in a year. The oldest and most unwell people sit next to the hallway door, so the tiger would probably drag one of them away. To protect one of us, all one hundred must now hold their respective bricks pressed against the floor. It is not only tiring but it’s also boring. Nobody wants to live like that. But what else could we do? Some begin to slowly look at the old men among us, wondering if they’re really worth so much to us. Does it make sense to sacrifice the quality of life for ninety-nine of us just to save one of our old men? It is amazing that this virus has placed this type of doubt in front of us in the 21st century. Our response to the crisis will, in fact, reflect the value system of our society.
Still, everyone wondered how long we should keep this tiger pressed under the net and how to get out of this situation. Someone then remembered that vampire. If the tiger was accidentally bitten by the vampire on the way to the ground floor, then at sunrise, the tiger could simply disappear when it was illuminated by the sun. This is analogous to the disappearance of coronavirus when the warmer weather arrives. So, it seemed reasonable to endure it for at least some more time. Then one of us asked the person next to them to press down their brick with their free hand, while they try to load their rifle, with which they could simply kill the tiger. That would be an analogy for the discovery of a vaccine for this virus. Another, however, also freed himself and began to develop a fluid that would kill any appetite the tiger had. Then the tiger would leave us all alone and just walk away outside. This would be an analogy for the COVID-19 drug, which would reduce the need for respirators for the seriously ill and relieve the pressure on the health system.
Suddenly, there seemed to be as many as three options - the disappearance of the tiger at sunrise, the loading of a rifle, or the development of a fluid that would kill the tiger's appetite. The problem is, there can be no certainty that any of those measures would work. During this time, the people are less and less attached to the net. If only two or three loosen their grip in the same place, the tiger will crawl out from there, and then it would once again need to be caught in the net. However, more and more people, eager for a normal life, are beginning to wonder whether it’s better to gamble with the 99 percent chance that the tiger will not grab them than to live like this, crouching down on the floor and pressing the net against the floor with everyone else. This is especially the case for younger, faster and more adept people.
But suddenly, an engineer comes up with something else. He teams up with the miner next to him. They ask those next to them to hold down their bricks with their free hands, and they go out into the hall. The engineer instructs the miner to dig a tunnel under the corridor, which would lead back into the forest. During this time, he places ten tiles instead of the hall floor, each of them with a sensor. He installs a laser beam on the ceiling, which alternately illuminates one of these tiles. If the beam is directed at the tile sensor and the sensor doesn’t register the beam, it means that there is probably a tiger sneaking onto those tiles. Then the tiles will collapse and the tiger will fall down into the tunnel, and will have to go back into the woods and he’ll need to sneak up on us again from scratch. If the tiger ever manages to get through such a security system, we still have a rope with a bell at the end of the hall. It will alert us to the fact that he has broken through that defense and then we will catch it once again in the net. But in the meantime, we will at least be able to live more normally and continue to do our work, regardless of the fact that there is a tiger outside our building. When the system is installed and tested, we will push the tiger out together with our net, then allow it to keep falling through the floor tiles, let it fall into the tunnel again, and then return to the forest. That's how coronavirus testing works, roughly.
There is only one thing to remember in any epidemic: we need to do everything we can to find out who is infected and who isn’t, and then physically separate the infected people from the healthy ones. This should be done among the population, but especially in hospitals, where the virus poses the most danger if it can enter them. Since coronavirus has entered several of our hospitals, anyone considering the complete relocation of all COVID-19 infected people from all hospitals to reception centres, to new hospitals, which is what was done in Wuhan, has my full support. Every action of separating the infected from the rest of the population makes it impossible for the virus to spread further. The most important thing is to prevent it from spreading to uninfected hospital patients who are most at risk.
If we can be that active in finding infected people and isolating them and their contacts, we will significantly slow down the spread of the virus. This virus is currently spreading at a tremendous pace as each infected human can transmit it to two, three or even four healthy people with their next step. But if, by taking an active approach to finding infected COVID-19 spreaders who don’t yet have symptoms, and by constantly separating them and all of their contacts and putting them into self-isolation, then we manage to get to a situation in which one infected person manages to infect, on average, less than one healthy person, then we are all pretty safe. The epidemic will slowly go away on its own, and the vast majority of us will be able to live relatively normally. The minority, on the other hand, will constantly rotate in isolation.
With proactive testing, for example, by small epidemiology teams that will go to the households of everyone who reports having symptoms and test them and then isolate them and their contacts if they’re positive for the virus, we will allow the vast majority of the population to live safely with the virus. I would definitely recommend the daily testing of all staff at hospitals, dispensaries, health centres, as well as people employed in retirement homes, as there will also be an enormous amount of damage if a COVID-19 epidemic develops in those places.
In addition to actively seeking out, testing, and then isolating infected people and their contacts, there are two other elegant ways by which we can further protect ourselves. The first is to build some kind of "safety net". We could define a very representative sample of Croatia's population of about 10,000 people, and test them once a week. In this way, we would make sure that the virus isn’t "sneaking" behind our backs and escaping into exponential growth in some part of Croatia.
Namely, when we quarantine, it will be possible for mini-epidemics to break out anywhere in Croatia. They, as we’ve seen in Italy and some other European countries, can grow very quickly to very large numbers of infected people. With this "network" that we would regularly monitor, we’d know that our virus isn’t spreading anywhere in Croatia, and we’d also know how many Croats are infected. Another approach we could take is to start looking for people with antibodies, who apparently have become infected with coronavirus, even though they aren’t aware of it, and then issue them passes and include them in normal life in important roles. However, we will still have to wait for solid scientific proof that immunity against this new coronavirus is indeed permanent.
Virus testing is somewhat comparable to counter-espionage in war. We’re confronted with an enemy who is invisible, and we only become aware of the effects of its actions a week later. In the meantime, we don’t know where the virus is and what it is doing behind our backs. SARS and MERS were significantly easier to control because the infected didn’t transmit the virus before the onset of coughing and other symptoms. With coronaviruses, the infection spreads during the incubation period, while the infected don’t have any symptoms yet, which is a big problem for us. But we can at least resolve it, somewhat, with more active testing.
If we allow it to, the virus will jump from the first infected person to two or three more people, then from each of them to two or three people again, and then do so again. That way, if the first infected person is drawn at the bottom of a piece of the paper, the wider and denser ‘’canopy’’ of infected people is constantly spreading over them, step by step. Through active testing, we’re able to find those who are infected among us. So, we constantly prune that "canopy" to make that situation as rare as possible. If the canopy ceases to spread from step to step because we constantly cut branches wherever we reach, then we’re in coexistence with the virus. We slowly get vaccinated, we treat the seriously ill, and there are fewer and fewer people who don’t have immunity for the virus to be able to jump on.
This way, one can live with the virus present in the environment and thus control the epidemic. What the Director of the World Health Organisation, Dr. Tedros Adhan, tells us is that we must not constantly be on the defensive, in quarantine, and wait for people with symptoms to report for testing. That would mean we're constantly behind the virus. The enemy will then constantly surprise us and strike us from somewhere. That's why it's important to test people as much as possible, but cleverly and reasonably so, and with clear goals.
Quarantine, simply, cannot be a longer-term solution to fighting the virus in Croatia. Initial estimates suggest that about half of Croatian private sector companies cannot withstand this situation for more than a month, and another 43 percent won’t manage for more than three months, which is a terrifying fact. Their exhaustion will also see the end of the filling up of the budget through corporate income taxes, so, there will be no funding for public sector wages either. This will mean that most people now sitting in their homes will no longer be able to buy food, and soon there will be no food to buy, either.
In addition to testing, there are a number of innovative approaches that we may need to resort to in order to be as safe as possible from the virus and escape the Italian scenario of exponential growth. For example, we might initially switch to a work week where people living in house numbers ending in 1 or 2 work on Mondays, those with 3 or 4 on Tuesdays, those with 5 or 6 on Wednesdays, those with 7 or 8 on Thursdays, and those with 9 or 10 on Fridays. This would turn the Croatian population into a so-called "metapopulation", that is, they’d be divided into five smaller non-contact populations. This is similar to a ship or submarine that is internally divided into bulkheads, so they can protect it from sinking if the hull breaks somewhere. That way, we would protect ourselves if the virus somehow triggered an epidemic within one of these populations, it couldn’t then spread to the other four fifths. Perhaps a two-day Monday-Friday work week for everyone would work in an even better way, as it wouldn’t allow the virus to spread day by day, and would still allow us to return to having nine working days a month, with additional work from home where possible. Perhaps even a "one week work, three week quarantine" option would be effective and safe.
The combination of all of these measures: (i) the continuous, active detection of infected persons and their separation; (ii) a "safety net" of 10,000 people for continuous nationwide testing; (iii) splitting the whole of the population into fifths, or working twice a week, on Mondays and Fridays; (iv) various measures to avoid social contact, such as banning large public gatherings, recommendations on wearing masks and gloves, and restrictions on travel and quarantine for arrivals from abroad; and (v) various innovative technological solutions, such as applications that inform all residents of the status of infection of people they have in their contact list, all of which seem feasible. This would probably protect us enough from the virus and allow the vast majority of people to continue, more or less, with normal life as much as possible. Because we need to get out of this quarantine situation as soon as possible and we need to make plans now.
Perhaps this unusual situation will be a historical reminder to both countries and individuals of the importance of self-sustainability and independence from others. It may be that many people in the world left without work because of the economic aspect of this crisis are encouraged to consider moving to cottages or to villages. Now that wireless internet can be accessed everywhere, it doesn't matter where the person on Earth actually lives. But if he has his own garden and his own well, at least he won’t get into the kind of awkward situation that many are now finding themselves in recent times. Perhaps one of the consequences of this crisis will be some new idea of organising the lives of individuals and countries, based on self-sustainability. This would also make Croatia, in general, a more robust country in the face of a number of possible new challenges of the 21st century.
Coronavirus will cause losses for humanity in 2020 on the one hand, but it will reduce those same losses on the other. For example, it will reduce the number of traffic accidents, the number of victims of violence, and deaths from polluted air. In addition, until yesterday, spears were breaking around every percent reduction in fossil fuel use, and now all of a sudden this reduction is forced and massive. In a rather improbable way, this pandemic at least helps combat humanity's climate change problem. In Zagreb, however, self-isolation due to the COVID-19 pandemic saved perhaps tens of lives of people who would have perished during the earthquake. If I paid for a ticket to watch a movie with such a scenario, i.e. an earthquake that affects people who are quarantined by a pandemic, so they can no longer be outside or inside, I would feel cheated. But, as the Chinese proverb goes, "There are countless things that cannot be imagined, but there are none that can’t happen.’’
This text was written by Igor Rudan and translated by Lauren Simmonds
For rolling information and updates in English on coronavirus in Croatia, as well as more articles by Igor Rudan - follow our dedicated section.
Igor Rudan: Why We All MUST Stay Home for At Least One Month
As Igor Rudan/Vecernji list writes on the 23rd of March, 2020, if we don't go into quarantine, our healthcare professionals will not have to worry about a few dozen or several hundred people who are suffering from coronavirus more severely, which our system can handle, but several thousand of them, which it can't. All of those differences are now our responsibility.
I have joined forces again with our renowned mathematician, Toni Milun, to explain through this text and the accompanying video why we now all have to stay in our homes for at least a month and strictly adhere to the quarantine guidelines.
Pandemics, like the world wars, are dynamic events with an uncertain outcome. In these times, things can quickly change from stage to stage. When encountering a new, unknown and invisible opponent such as this coronavirus, surprises are always possible. That's why one should be careful, but one shouldn't panic. Only those with ''cold'' heads can make all of the important moves and respond to challenges at the right time, based on reliance on science and proven information.
On the one hand, the virus can always surprise us with its mutation. Random mutations of its genetic instructions can change the severity of the symptoms it will cause when causing an infection. They can also change the rate of its spread among the population. On the other hand, there are several lines of defense at our disposal that, depending on the behaviour of the virus, can be activated at the right time. Compared to the situation only three weeks ago, today, I have to make it clear that the epidemiology profession has significantly changed its perception of the danger of this new coronavirus.
By constantly collecting information from many countries, we now have a better understanding of the way it threatens us. I will try to explain here why the attitude of the profession has changed and why everyone now really MUST stay disciplined in their homes for at least a month.
I've written before that this is already the seventh coronavirus to try to adapt to the human species. The first four cause common colds and have been harmless to humans. The fifth, the SARS epidemic, however, was terribly dangerous. It killed as many as 10 percent of the people it infected. It expanded in 2002 from the Chinese province of Guangdong to more than 25 other countries, but was stopped everywhere on the front line(s) of defense.
The sixth one, the MERS epidemic, was even more dangerous. That killed as many as a third of those infected. It spread from Saudi Arabia to more than 25 other countries. But even then, it was stopped by the front lines of defense. These lines of defense include the isolation of patients and all of their contacts. When the epidemic of the seventh coronavirus, with COVID-19 as its causative agent, erupted in Wuhan in January 2020, it isn't surprising that the epidemiologists' interest was primarily focused on the death rate among those infected.
The reason is that previous death rates for SARS and MERS were so terribly high - 10 percent and 35 percent, respectively.
It was soon realised that the death rate among the most severe cases and hospital patients in Wuhan was about 5-10 percent when it came to this new coronavirus. However, it was only valid for the most severe cases that came to the hospital there, but not for anyone infected in the community. Infected doctors, like most patients in the population, had significantly milder issues. Therefore, it was necessary to determine as soon as possible the rate of death among those infected.
We got our first idea of the actual death rate of infected people when the work of Z. Wu and J.M. McGoogan was published in JAMA back at the end of February. It was based on a major report by the Chinese Centre for Disease Control, based on 44,672 COVID-19 positive patients in all Chinese provinces.
The authors showed that the death rate in the Hubei province was 2.9 percent, but they knew it was unrealistically high. This is because, at the earliest stage of the epidemic, the overwhelmingly severe cases that came to hospitals were tested, and there was no time at the height of the epidemic to test many in the community. A much more realistic estimate, therefore, was among those who tested positive outside the province of Hubei, on the front lines of defense of all other Chinese provinces. This death rate was 0.4 percent.
This means that for every 200 people with COVID-19, if given adequate medical care, only one person would die, or even less than that. Confirmation of that came from South Korea, where an unusual incident occurred. A community epidemic happened there, behind the front lines of defense. The authorities there went forward with en masse testing. Thus, the path of the virus among the population was constantly monitored and all the infected were isolated.
For such a very deep first line of defense, South Korea also had enough money, experience and all the other necessary facilities. 10,000 people were tested daily. Based on the first 140,000 tests, the rate of deaths in the community was estimated to be about 0.6 percent, again - one in two hundred, and quite similar to the estimate for all Chinese provinces outside of Hubei. These two figures are also very close to the estimate I made on March the 1st, that is, when spread among the community, COVID-19's death rate should be between 0.5-1 percent.
In addition to the death rate among all those infected, it was also important for epidemiologists to know what the chances of a cure for all those who end up in hospitals are. It's important to evaluate these prospects when the patients aren't treated in the face of a booming epidemic and during an overload of local hospitals, and the situation in which entire medical teams are infected, but in conditions of being well prepared.
We learned these outcomes from the work of W. Guan et al., Published in the NEJM magazine. On February the 28th, they released a series of 1099 patients with laboratory confirmed COVID-19 infections from 552 hospitals in 30 provinces in China. This was a representative pattern of hospital treatment outcomes for China, in an environment where adequate care could be provided to all those infected. The estimated mortality rate of those with COVID-19 who end up in hospital was 1.4 percent, which was indeed much less than the first experiences in Wuhan.
Based on these two key pieces of information about COVID-19 - that is, in the community, it can lead to the death of only one in 200 infected people and that it kills one in 50 to 100 hospitalised people in hospitals - the epidemiology profession had its breath taken away. It no longer seemed to anyone that we were dealing with such a dangerous infection here. This is evidenced by the reactions of the world stock exchanges: Dow Jones was at 24,720 points on February the 28th, and jumped to 27,087 points by March the 3rd, meaning that it gained 10 percent on the total value in just five days after mortality rates became clearer.
The reason is that stock market investors have been in constant contact with leading epidemiologists over recent days. They were interested in how the situation was developing hour by hour. The view of the epidemiology profession during those five days was that we were likely to suppress the COVID-19 pandemic soon. These were exactly the days when I found myself in Zagreb and gave my first estimates to the Croatian media, after the first COVID-19 patients were recorded here.
The epidemiological profession's view at the time was that the primary epidemic, in the City of Wuhan and in the province of Hubei, had been in continuous decline from February the 8th until the end of February; that the first lines of defense were able to stop the virus in thirty Chinese provinces, each with tens of millions of inhabitants; then that the virus was successfully halted on the front lines of defense in Japan, Taiwan and Singapore, the countries that have the highest human traffic with China.
In addition, even in South Korea, where an unforeseen epidemic occurred in the community, it was managed by intensive testing, with as many as 10,000 tests carried out per day.
The developments were then completely similar to the scenario already seen with SARS and MERS. The same scenario was repeated during the transition from February to March and with the third coronavirus, caused by COVID-19. There was also a primary focal point in the City of Wuhan in the Hubei province. It was suppressed by a large and strict quarantine, as the ultimate line of defense. All secondary foci were controlled by primary lines of defense. None of the epidemiologists thought at the time that EU and US countries wouldn't be able to stop it in the same way.
The epidemic then seemed practically to be extinguished, and even the World Health Organisation delayed declaring COVID-19 a pandemic at all. It did it only about ten days later, that is, on March the 11th, because things had changed to such a dramatic extent. What, then, changed so much between the period of February the 28th and March the 3rd, when the epidemic seemed practically overpowered, and March the 11th, when the World Health Organisation declared a pandemic and the need for the absolute highest degree of caution?
According to the current understanding of the situation that the epidemiology profession can offer, after celebrating the Chinese New Year on February the 12th, about a week later, a number of Chinese workers employed in their textile industry, in northern Italy, returned to Italy. They were tested and recorded at the Italian airports by "first line of defense" measures. However, this seemed to be heard among the Chinese, so many began avoiding direct flights from China to Italy, returning via other European airports that didn't exercise such strict controls. The Italians, however, didn't control flights from the EU. Because of this, an epidemic that no one knew about began to quietly spread in the smaller cities of Lombardy, where many Chinese workers live, and behind the Italian line of defense.
There are many people living in northern Italy who went skiing in late February and early March. Across European ski resorts, they spread the infection enormously to the Swiss, French, Austrians, Germans and Spaniards, as well as citizens of many other countries in northern and western Europe. This is probably also because the spread of coronaviruses is generally favoured by lower temperatures. The current picture of the spread of the epidemic and of the hardest hit countries is in line with these developments.
As I described above, from March the 3rd to the present in many EU countries, most notably in Italy, which was one week ahead of the others, the number of infected people started to increase at an incredible rate. If the virus breaks through the first line of defense, we know that its growth will be exponential, but the human brain can hardly understand what that really means. In linear growth, anything added in the fifth week of expansion will represent one fifth of all cases so far. In the tenth week, a tenth. We know that and it is logical.
But when it comes to exponential growth, everything added up in each coming week will account for the vast majority of all cases, and anything that has happened before will seem irrelevant compared to just one week previously. This is what Tony Milun explains in today's video.
I wrote about the dangers of exponential growth and the need to introduce major quarantines in Europe on March the 8th, and offered the option of strict quarantine for Croatia on March the 12th. But I have the impression that even in mid-March, the leaders of some EU countries still didn't understand what the real danger of COVID-19 was. Thus, this coronavirus doesn't kill primarily because COVID-19 is medically particularly severe in most patients, but mostly because it spreads deliberately and rapidly among humans.
Because of this, this coronavirus is incredibly fast in generating a huge number of patients, about 5 percent of which end up in an extremely serious condition. If we were able to provide each of them with optimal care in a timely manner, almost all the seriously ill would be saved. But if everyone gets sick at the same time, we can't give them all intensive care. That is why almost all of the severe coronavirus cases will die. This is the way this virus has been killing so many people in Italy. They could have tens of thousands of patients suffering severely who will not be able to have access to intensive care and respirators.
The reason for the deaths in Italy was not, therefore, the severity of coronavirus per se, but rather that no one had taken the danger of an exponential spread seriously, meaning that quarantine was declared too late and then people just failed to respect it.
The incredible spread rate of this coronavirus is shown in the example in this table (below). The table shows what is happening to the population when the number of new cases is increasing by about 26 percent day by day compared to the previous day. This is quite a realistic scenario for many European countries these days.
The table first shows the days since the epidemic began. In the second column, the number of those infected with the virus is shown. It's important to understand that those infected with the virus have not yet been discovered because they do not yet show any symptoms. Nonetheless, they can spread the infection over the next week while looking quite healthy. Only when they show symptoms of the virus a week later will they find themselves in the third column, as those who are "sick." This means that when testing the number of patients on any given day, that we should expect that the actual number of infected people in the population is already ten times higher.
DAY 0 = 1 INFECTED = 0 SICK
DAY 7 = 10 INFECTED = 1 SICK
DAY 14 = 100 INFECTED = 10 SICK
DAY 21 = 1,000 INFECTED = 100 SICK
DAY 28 =. 10,000 INFECTED = 1,000 SICK
DAY 35 = 100,000 INFECTED = 10,000 SICK
DAY 42 = 1,000,000 INFECTED = 100,000 SICK
DAY 49 = 10,000,000 INFECTED = 1,000,000 SICK
Croatia has now passed day 21 and is moving towards day 28, but has declared a quarantine on time. Most EU countries have passed the 35th day and only then did they declare quarantine, so they can expect as many as 10 to 100 times more infected people than Croatia can. Italy declared quarantine when it was nearing its 42nd day and probably already had hundreds of thousands of people infected.
There are several other interesting things about this exponential spread of this infection. Namely, small countries are still in more danger than big ones are. The virus will spread exponentially among people using their mutual contacts, at the speed shown in the table above. It doesn't matter how many inhabitants there are in the country in which it is expanding.
This is why smaller countries will be relatively more severely affected than large ones. For example, Italy, with its 60 million inhabitants, can spread the virus for 42 days, causing as many as 1 million people to become infected. Of these, about 5 percent, ie 50,000 of them, will become seriously ill. This is too large of a figure for their few thousand intensive care beds, and many cannot be provided with the assistance they need. Therefore, the Italian death toll from COVID-19 could be in the tens of thousands. However, not all the severely ill will die, because many will only require oxygen for their treatment and will not need a respirator.
This means that in Italy, as many as one million infected people could seriously endanger some 25,000 people. At least a few thousand of them will be assisted by intensive care, so the death toll would then be around 20,000. Even in such a scenario, it should be understood that only 1.6 percent of all Italians would get infected with COVID-19 at all, because Italy is a pretty large country.
In addition, 99.97 percent of Italians will survive it, which is important to understand for some future discussions on this topic. But, if COVID-19 had expanded exponentially in a much smaller country, it could have done significantly more damage there relative to the entire population, in relative terms. Things that happened in Italy should be put in an additional perspective. The scientific paper by A. and G. Remuzzi published in the March 2020 issue of Lancet showed that the average age of the first 827 deaths in Italy was 81 years and that more than two-thirds had diabetes, cardiovascular disease, cancer or were ex-smokers.
So these were the same people who probably would've died of the flu if they had not been vaccinated against it. Furthermore, in the scientific work of Rosan et al. Published in the 2019 International Journal of Infectious Diseases, influenza in Italy was attributable to 20,259 deaths in the 2014-15 season, and a total of 24,981 deaths in the 2016-17 season, even with vaccination. This means that the total number of deaths in Italy from COVID-19 could eventually be at least roughly comparable to those figures if the number of infected and dead continue to decline in the next few days.
However, taught by the experiences from back at the beginning of March, I'd also like to add that this is the view of the epidemiological profession on the state of affairs at the moment, to this day. Any new contingency - such as the realisation that the virus has indeed mutated and become more dangerous for younger people, or a repeated escape of the virus into an exponential spread, could change that view once again. Epidemics are dynamic and unpredictable events.
What we need to know now is that in the period from the 3rd to the 17th of March 2020, Croatia was still managing to maintain its first line of defense to a significant extent. It was at a time when the largest number of European countries already had exponential growth and uncontrolled spread in the community and reached a very large number of people with serious clinical issues that they would no longer be able to help. As you will see from the video by Toni Milun, in those fourteen days, Croatia had a 15-16 percent daily increase in the total number of infected people, while among the thirty other countries in Europe, Denmark was the worst with a 44-52 percent daily increase.
Then, after March the 17th, we introduced quarantine measures. If we're to believe the numbers, because of all that has been done, we'd have to deal with at least 10 times less severely ill people than other Europeans, and as many as 100 times less than the Italians. But that will only be valid IF you're all staying in your homes now and not leaving them for a month. If you ruin all the good that Croatian experts have done so far, which means with careless exposure and socialising in this situation, the virus will continue to spread rapidly among us.
Then, our health care professionals won't just need to worry about a few dozen or several hundred people with a severe clinical picture, which, yes, our system can handle, but a few thousand of them instead, which it just can't cope with. That difference depends entirely on us now. We need to remain patient in our homes for a month.
But then, just when everything was being done the right way, we were hit by this earthquake. I watched people go out into the streets after the earthquake struck, talking to each other in shock. Then, many people from Zagreb took the virus down to the south of the country with them, where we have significantly less capacity for intensive care. So, it was an incredible, totally incredible turn of events. Because of this, we can no longer predict the numbers. The number of infected people could be much higher than planned for by Croatian epidemiologists.
Instead of about 3000, it could now grow to a much larger number. All this is beginning to remind me of the finals of the World Cup two years ago. First, we played that game better than anyone could have hoped we would - that part would fit this period of "first line of defense."
We had the lowest percentage increase in the number of cases in 30 countries across Europe. Then, an unfortunate own goal happened - because, from various European ski resorts, but also through the emergency services, the virus still found its way into Zagreb's hospitals, exactly where we didn't want it.
But then the equalisation came - we "locked" the country down and declared quarantine at the right time, thus preventing a large number of infections. But then came the earthquake in Zagreb, people went out onto the streets, the virus spread through conversation with one another, and then people carried it south, where we don't have so much of a capacity for intensive care.
That's why we all need to be Subasic now, but this time we simply have to defend the penalty. And all you have to do is stay home for a month.
This text was written by Igor Rudan and translated by Lauren Simmonds
Make sure to stay up to date with our dedicated section for all you need to know about coronavirus in Croatia.
Igor Rudan: How Epidemiologists Used Numbers to Protect Croats from COVID-19
As Igor Rudan/Vecernji list writes on the 20th of March, 2020, Croatia was the country with the lowest percentage of newly COVID-19 infected persons in Europe during the two weeks from March the 2nd to the 17th, 2020, which means that our "first line of defense" did an excellent job and lasted the longest. Then we went into quarantine at the right time, at a much earlier stage of the spread of the epidemic than everyone else did.
Now that we have all become "Quarantine Croatia", yesterday, I joined forces with our famous mathematician Toni Milun to explain together just how we came to be in this situation at all.
In mid-January 2020, a number of friends from Croatia suggested that I start a new popular science series on Facebook in order to follow the COVID-19 epidemic in Wuhan. I called my Chinese colleagues at the time, asking them to briefly describe what was happening to them. They conveyed a few simple but very helpful messages to me. What surprised me the most was the thought of putting 56 million people in quarantine for an extended period. That, then, on January the 17th - so, just two months ago - sounded like a completely radical idea. But when I found out more, and then one week later - on January the 23rd and 24th - I saw that they'd indeed closed off Wuhan and fifteen other cities, I realised that it was an almost surreal event, one that was certainly worth watching. Thus, on January the 29th, the ''Quarantine Wuhan'' series of texts began.
My Chinese colleagues told me that more and more people with some sort of unusual pneumonia began to show up at Wuhan's huge hospitals on a daily basis. That would usually drag on on for about ten days without responding to any sort of antibiotic therapy.
Some people soon required additional oxygen or mechanical support to help them to breathe. If the doctors themselves became infected, the fear would grab them. How could it not? It was an unknown cause of pneumonia, and about one in ten patients would die even with hospital treatment. But what would surprise them was that the infected doctors had generally mild symptoms. They didn't understand how it was possible that these infected patients were in such a poor condition but the infected doctors seemed much better if the cause of their respiratory infection was the same.
The answer to that enigma, however, was hiding outside the hospitals, in the very streets of Wuhan with its eleven million residents. To epidemiologists, such a rift of symptoms was a clear signal that an epidemic had to have been spreading rapidly among the population of that city for some time. It can cause different symptoms in different people. In the vast majority of those infected, the symptoms will be mild or moderate, so they will never report to the hospital. Symptoms would be worse in about fifteen percent of people, and they'd require extra oxygen. Only the remaining five percent of those infected would end up in critical condition, in need of respiration and intensive care. They also noted that when doctors transmit the virus to other patients in the hospital, it also kills about one in ten people infected. Mostly those who already have other serious illnesses. Men, smokers and older people were the most high risk groups.
The doctors in the hospitals saw only that extreme part of the spectrum of the sick - serious and critical cases. Other infected residents, those with mild and moderate symptoms, walked around Wuhan normally. There, they spread the epidemic at a rapid speed. Epidemiologists in Wuhan realised that the new illness would therefore not kill every tenth person it infects, but maybe every 100th person, maybe even every thousandth.
The number of deaths in the hospitals could be used as a numerator, but all infected residents of Wuhan outside the hospital should have been placed in the denominator, ie, the numerous people with milder symptoms spreading it around. At the beginning of the epidemic in this city of eleven million people, no one knew if there were just a thousand, ten thousand, a hundred thousand or maybe a million [infected people]. So quarantine had to be declared. Most importantly, then, it was urgent to stop the exponential spread and then slowly explore what was going on.
It then became clear to them that COVID-19 was not an illness that primarily kills owing to the sheer severity of its symptoms. This was an illness that kills with an incredibly high rate of spread among the community. This spread leads to a tremendously rapid increase in the total number of infected people, and thus five percent of critically ill people, day by day. The critically ill people then cannot receive adequate care. That is why, for every deceased person who couldn't be saved, there are several others who probably could be, but they all came in for treatment at the same time.
This overloaded the hospital's intensive care facilities. My colleagues in China have told me that, after all the bad news from Wuhan, it will probably surprise us how relatively mild it is for most infected people, whether tourists or seafarers bring it to our area of the world. They told me that the illness itself should not feared, but its rapid spread should be. Therefore, three things are crucial to its control:
(1) The spread from China to other countries should simply be stopped by the "first line of defense" - the constant isolation of the infected people and their contacts. This approach had previously proved successful and stopped two previous coronaviruses, SARS and MERS, although both of them had managed to spread to more than twenty countries from China and Saudi Arabia. It was therefore likely that this would work for COVID-19.
(2) We must be extremely careful if a virus manages to break through the "first line of defense" by mere chance. That is when all those infected people with milder symptoms will start spreading it to the population very quickly, aided by the "super spreaders" that infect many individuals. Then the rate of increase in the number of cases can make anyone unpleasantly surprised and entirely unprepared.
The reason is that the infections we're confirming today reflect the spread of the infection days earlier, and not the current situation. Between the infection and the diagnosis of the symptoms, there is a period of "incubation", which lasts about a week. Therefore, if we diagnose 100 infected people on Saturday, we gain information about the spread of the infection since last Saturday. But during those seven days, the virus has spread rapidly, so today it has, in fact, infected more than 1,000 new people. But they will only become visible to us next Saturday. This is the problem of "silent", invisible, exponential growth, which isn't intuitive to the human brain.
In short, the actual current state of spread of the COVID-19 infection is always significantly worse for us, as the current number of confirmed cases indicates - about ten times worse. Therefore, if the virus breaks through the first line of defense, the key decision will be to declare quarantine as soon as possible so that the virus doesn't manage to escape and grow exponentially. And the effects of quarantine will not be visible for the next day, but only in a week's time. Until then, terrible losses will be suffered if a state of quarantine is declared too late, as is happening these days in Italy.
(3) Of course, we must take great care to prevent the virus from entering our hospitals or nursing homes, as it can create a huge amount of death there among patients who are already impaired. These three points are the standard epidemiological measures of protection, so it was quite clear what to do when COVID-19 knocked at our door. I began to closely monitor the results of the quarantine effect in Wuhan, but also a comparative increase in the number of cases in Europe, and Toni Milun showed how that works in a video.
The most important day of this COVID-19 pandemic, at least so far, was probably February the 8th, 2020. Thanks to several consecutive days of declining infections in Wuhan, it became clear that the epidemic in China was beginning to wane and would virtually be extinguished over the coming weeks. It was great news for all of us. That meant that the COVID-19 epidemic could be suppressed even if the virus broke through the first line of defense.
From that February the 8th until February the 21st, things were constantly getting better globally. The number of newly infected individuals in China had been steadily declining. China's surrounding countries, already taught by experience with SARS - Singapore, Hong Kong and Japan - "caught" the virus from China in their first line(s) of defense. They controlled it with a stricter regime along borders, with frequent testing and the isolation of the infected and their contacts. They didn't even need a quarantine, the first line of defense measures produced results.
Furthermore, with the exception of three cases in Australia and one case in Argentina, there were no recorded deaths from COVID-19 in the entire Southern Hemisphere. It gave us all a huge amount of hope that COVID-19 would actually prove to be a seasonal virus and disappear from the Northern Hemisphere with the arrival of late spring and summer. And in Europe and the US, very rare cases were easily ''captured'' by the front lines of defense.
Since February the 21st, however, South Korea and Iran unexpectedly came into focus. The first country had a really awkward incident, which I'll describe in one of the following sequels as an example of another successful way to fight this virus. They were able to extend their first line of defense without quarantine. On the other hand, very little was clear about Iran. I was worried that this country could eventually become the biggest problem with COVID-19 because it was the first less developed country in which the virus began to spread freely. On the positive side, however, Iranian epidemiologists are very adept at combating infectious diseases.
I also noticed that Italy jumped from 3 to 20 cases on February the 21st. I thought, maybe it's some group travelling together. But on a day-to-day basis, on February the 24th, Italy already had a total of 229 infected people, while other European Union (EU) countries had only a few cases and controlled that with their first line(s) of defense.
When I landed in Zagreb four days later, on February the 25th, Croatia discovered its first infected citizen after they were tested. Italy, just across the ''way'' from us, already had 322 infected people by then. The virus had already penetrated their first line of defense by then, so I expected that they would declare a quarantine for at least Lombardy the next morning.
If they'd already registered 322 infected people, it meant that the population was already significantly more infected than that. However, the situation in all other EU countries was still calm. The first lines of defense in the EU were expected to successfully control the entry of the virus. One country can always be isolated from another if that is needed, and Italy is pretty well isolated anyway. I was hoping, in fact, that my colleagues in Italy would have additional reports from China, so they probably calculated their hospital capacity and knew what they were doing. I assumed that they wanted to preserve Italian tourism and the economy for as long as possible and prepare people for quarantine, which they'd obviously have to declare as the first in Europe.
In Zagreb, therefore, I was really amazed by the panic that gripped people when they heard that our first case had been recorded here. I knew that our first line of defense could easily deal with sporadic infections, and globally the situation was getting better day by day. For epidemiologists, the most important of all indicators was the transition of the exponential growth of all newly infected people, from the onset of the epidemic in Wuhan, in a linear way, which was greatly slowed down. It was exponential until about February the 17th, and linear from February the 17th to March the 1st. After this "linear" period, the epidemic is expected to enter into a final stage, ie - a curve alignment and then a decrease in the number of new cases. Tony explains that nicely in a video, too.
All of the available data at the time fueled the real hope that the virus was indeed seasonal, and that the first lines of defense of all developed countries would successfully stop it. We knew then that just about all Chinese provinces had already stopped it, from which it had expanded from the Hubei province, to some thirty of them. Japan, Singapore, and Hong Kong had also succeeded. So why wouldn't it be stopped by the EU and the US?
Owing to all that, panic in Zagreb didn't really seem appropriate to me. As my return coincided with the first recorded case, the cameras of many televisions ''stumbled'' upon me unexpectedly during a guest appearance at Edward Bernays, where I gave a lecture upon invitation. At that time, I tried to appease all of the journalists, as well as the general public, knowing that all epidemiological measures were functioning globally, that the virus was already under control in China and held back by the front lines of defense elsewhere.
When asked what kind of ailment was approaching us, I compared it to "more severe flu, but for which we don't have a vaccine." As an epidemiologist, I knew that severe flu alone was equal to about 650,000 deaths a year, and without a vaccine, well over a million.
It didn't seem to me that COVID-19 could ever reach those figures, given that it had been effectively halted in China at less than 5,000 deaths, and elsewhere the situation was quite calm. But what I wasn't aware of was how little of a danger people in Croatia associate the flu with today. Unfortunately, this misunderstanding still follows me around in many conversations with people today. Then, on March the 1st, I explained on Sunday at 2 that you really shouldn't panic in Croatia, because unless the virus mutates, it can hardly endanger more than 0.5 percent to 1 percent of all infected people.
That it will not endanger the younger age groups, but mostly those over fifty years of age. And it can't even infect us all, because infecting the entire population must also be self-limiting at some point when collective immunity is acquired. With all these predictions, nothing has changed to this day. After that show, however, completely incredible things began to happen, like from something out of a nightmare designed for an epidemiologist.
First, on March the 3rd, WHO Director Tedros Adhanom announced that the COVID-19 death rate so far had been 3.4 percent. This was not inaccurate in any way, as he listed it as the death rate among all positively tested people but not all of those who were infected. Therefore, it wasn't useful information to the public. Specifically, the figure is a combination of the death rate of hospital infections among the elderly and sick from Wuhan and Italy, which was as high as 5 to 10 percent, and the death rate when the virus has spread in the community, which is typically about 0.5 to 1 percent. Therefore, it isn't actually representative of either situation.
But how do you explain to anyone now that the director of the World Health Organisation in Geneva doesn't understand how confusing it is for the concerned public to quote such a figure, perhaps five times the one that is really more applicable? To make matters worse, he was first opposed by US President Donald Trump. He called that number "wrong," and he was largely correct in doing so. Suddenly, it put me in a situation where I had to explain to many that I wasn't underestimating the danger of COVID-19 when I said that the death rate, applicable to the whole population, could be 0.5-1 percent. And next to me, opposite to the director of the World Health Organisation in Geneva, was Donald Trump alone. No wonder the people who trusted me the most were already quite mad at that point. Fortunately, many other experts came forward over the next few days, confirming the estimates of 0.5-1 percent.
Thus, the days of March the 5th to the 7th were spent trying to explain the applicable rate of death, in three consecutive posts. All of this at least served as a great article in Index.hr with answers to 20 questions about COVID-19, which, I hope, helped many to understand more about the threat we're facing and reduce the noise. However, in these discussions, of course, I kept looking into the numbers of newly infected people around the world through the corner of my eye.
Suddenly, not only was the situation in Italy no longer clear to me, but the situation in the whole of Europe became a blur. What is everyone waiting for, why don't they declare quarantine? On Saturday evening, March the 7th, Austria already had 79 cases, Sweden 161 cases, Belgium 169 cases, Switzerland 268 cases, Spain 500 cases, Germany 799 cases, France 949 cases... and Italy had 5883 confirmed infected people?!
I looked at all these figures and I was deeply concerned - but I just couldn't believe the Italian situation. It has been revealed that they already had at least 60,000 people spreading the infection around, and that number was to grow exponentially for at least another ten days, even if they were to have declared quarantine the very next day. In any case, it was then quite clear that everyone in Europe would have to be quarantined, regardless of the fact that we in Croatia were still holding up with our first line of defense.
The next day, on March the 8th, Lombardy was quarantined, but the news leaked to the media too soon. Numerous students fled to the south of the country, spreading the contagion. The whole of Italy was then quarantined. On the same day, March the 8th, I explain in my post "The Justification of the Huge Quarantines" and the problem of exponential growth in numbers infected as a key problem of the COVID-19 pandemic.
It was already quite clear by then that we'd be quarantined in Croatia in a few days. I started counting when it would be best to declare a quarantine in Croatia. I estimated that the first major jump from 10 to 20 infected people would be a good time. The number of infected people who were suffering more could then, with a little luck, see it stop at figures where our health system would have a good chance of helping everyone, with a truly minimal number of serious cases of infection.
That jump, from 14 to 19 infected people, happened on March the 11th. At 3:00 on March the 12th, I immediately posted a status entitled "Contrast is the mother of clarity", explaining that we now have the option to either quarantine very strictly for the next 30 hours and then cure the severely ill as they emerge or let the virus spread to save the economy and preserve normal life, but also prepare for a fair number of deaths. I knew that our epidemiologists were looking at these figures and thinking about them, so I wanted to give them the support from science that they weren't wrong. It is, however, a completely unbelievable decision to invite the whole nation to temporarily self-isolate.
In our case, that decision was further complicated. Namely, we're holding the rotating Presidency of the European Union and we have only 19 infected people, and we could close our borders. Other countries, however, have hundreds and thousands of infected people, numbers that are growing exponentially, but they aren't even thinking about such a move yet. I was pleased to see that as early as Friday, March the 13th, a decision was made to close the schools, sending a message to the population that Croatia was withdrawing into self-isolation.
We locked our country up exactly when we needed to, so we shouldn't have too many infected now, and again, Toni Milun assesses the details in his video. Toni and I joined forces today to show that Croatia was the country with the lowest percentage increase in newly infected people in Europe during the two weeks of March the 2nd to the 17th, which means that our "first line of defense" did a great job and endured for the longest period of time.
Then we went into quarantine at the right time, at a much earlier stage of the spread of the epidemic than everyone else. This has already prevented a very large number of infections so that we don't have to treat them. It has helped us in all steps with the legacy of the great Andrija Stampar, but also with our relatively recent war experience that EU countries don't have. But if anyone thinks this is the end now, I'm afraid he's living in fantasy land. This is just the end of the beginning.
****
Translation by Lauren Simmonds, Editor of Total Croatia News.
For the latest on the coronavirus in Croatia, follow the dedicated TCN section.
Croatian Scientist Igor Rudan Talks Chinese Anti-Coronavirus Measures
Prominent Croatian scientist Igor Rudan writes exclusively for Vecernji list on the 18th of March, 2020 about coronavirus, and in his latest article, he discusses how the Chinese are managing the coronavirus epidemic so well.
We are transmitting Igor Rudan's latest article in full:
''In my article on the spread of COVID-19 written for Vecernji list three days ago, I tried to explain the danger we're facing.
I've clarified the two main ways that the virus can put us at a greater risk - its rapid spread in the community and hospital outbreaks. I also explained behaviours that should help in both cases. I concluded that Croatia had well prepared defense lines, which in the first weeks, had yielded measurable results in relation to the environment. However, I also emphasised in this text that "... with epidemics, things can quickly turn against us just because of a little carelessness or the irresponsibility of individuals, and in just 48 hours, from a successful country, because of just a few incidents, things can change.'' and then every country quickly starts being followed case by case.
Unfortunately, three days later [after that article] we're witnessing just how important this warning was. Doctors at several leading Zagreb hospitals are now infected with coronavirus. More than a hundred health professionals and their contacts, are therefore isolated. Several Croatian broadcasters have mentioned individual negligence as a possible cause, although all epidemiologists have been calling for caution for at least a month, and all of our doctors are well aware of the risks of viral outbreaks. Thus, despite several weeks of professional efforts, the start of the fight against coronavirus in Croatia could be marked by hospital outbreaks. Obviously, the words of the 19th-century Prussian military strategist Helmuth von Moltke, who taught us that "no war plan will survive its first contact with an adversary,'' are still true to this day.
It's less evil at least that such a failure occurred at such an early stage. Now, clinicians in hospitals will also raise the level of severity to that shown by public health professionals for weeks. In addition, hospitals are still not significantly burdened with infected patients. Furthermore, sending more than a hundred health professionals into self-isolation will allow them to rest well, so we'll also get a backup squad. This may be absolutely necessary in just two weeks, provided that the number of cases of new patients continues to increase significantly in Croatia and that the frontline doctors themselves become infected.
At present, however, the issue of how many patients in hospitals may have been infected is of the greatest concern. We'll know this within a few days, when their incubation period is over and some may develop COVID-19 symptoms. Infected Zagreb hospital patients could become the first Croatian cases to create a more severe clinical picture, but still a curable one. Hopefully, there will be as few of them as possible, and that everyone will learn valuable lessons from this early incident.
By now, coronavirus has spread to so many countries that some entry and defense models are beginning to crystallise - such as the Chinese, South Korean, Singaporean, Iranian, Italian, German, French, Spanish and American ones. In the past few days, I've often wondered which of these models will most closely resemble the situation in Croatia, in order to contact my global health colleagues there and seek their advice, since they are all ahead of Croatia in terms of the epidemic.
We can see now that the onset in Croatia could be marked by the initial spread of contagion in major hospitals in the capital. This situation is most similar to what was happening in Wuhan, where the pandemic started. So I called a few colleagues from China, leading global health experts there, to ask them to recall all the contingencies and "bottlenecks" they had to deal with while fighting the Wuhan epidemic. I told them that the Croatian, ie the Dubrovnik invention from the end of the fourteenth century - quarantine - saved Wuhan and China from COVID-19 in the 21st century, and that it would be nice if their experiences would help us here in Croatia now. So, I'll relay their story of Wuhan, which may also carry some useful advice for us.
In November or December 2019, somewhere around Wuhan, a new coronavirus managed to transfer over from a small mammal, a bird or a bat, to a human, and then spread for some time to the local population. After several hundred infected people, severe cases of pneumonia occurred, predominantly among older men. They ended up being treated at the hospitals of Wuhan, with eleven million residents.
Nobody even noticed those isolated first cases as something special. It was only between December the 26th and the 28th that the first group of patients with this unusual pneumonia appeared in the same hospital. It was the "Hubei Hospital for Integrated Traditional Chinese and Western Medicine" (HICWM). All of the patients had stories that were in some way related to the Huanan Fish Market. It was then that the doctors at that hospital first suspected that it could be a new pathogen. But the doctors were already infected by then.
Moreover, they infected many of their colleagues at a rapid speed, and they in turn infected their patients. Many patients were already seriously ill, those who were old and those with compromised immune systems. Everyone was aware that a new contagion was spreading, but its symptoms were generally mild in doctors and younger patients, but more severe in the elderly. Lung inflammation would occur relatively infrequently, and no one knew what was causing it, but it was extremely dangerous for the elderly and the sick. On the last day of 2019, the Chinese authorities informed the World Health Organisation in Geneva of the situation and closed the fish market on the first day of 2020.
However, it took time to isolate the virus from the blood of those infected. The virus was discovered on January the 7th, 2020 and was immediately recognised as a new, seventh human coronavirus, somewhat similar to SARS. It was shared on the 12th of January, 2020, with the whole world. On this basis, diagnostic tests were available as early as the next day, and we were finally recognising who was infected. The problem with the new coronavirus was that it spread rapidly and successfully among people in the phase until the infected showed symptoms, so it was clear that an explosive epidemic across Wuhan was inevitable.
During that time, between December the 26th, 2019, and January the 12th, 2020, the coronavirus epidemic spread rapidly across Wuhan, and a large number of doctors in hospitals became infected with the virus. Although their clinical picture was neither problematic nor personally threatening, they wanted to continue helping their patients, but they shouldn't have done so. Specifically, they were able to transmit the infection to people in much worse shape than them. Entire medical teams had to go home to get over COVID-19 or quarantine their colleagues' contacts. In those days, when there weren't enough doctors in Wuhan's hospitals and the epidemic spread among severe hospital patients, most people died in Wuhan. The death rate among the already old and severely ill patients was, of course, much higher than it would be among the healthy population outside the hospital.
Around January the 15th, the number of newly infected people in Wuhan was already close to 500, and on January the 19th, it was close to 1000, reaching 2200 on January the 22nd. But the problem with the outbreaks is that these patients went to hospitals and were tested there days later. Thus, epidemiologists were only able to notice this "jump" from 100 to 200 newly infected people in hospitals on January the 22nd.
This was a sure sign that the epidemic was already spreading rapidly among the population. This is important to remember, because it means that when around 200 infected people are tested today Europe, it means that the actual number of newly infected individuals among the population on that day is probably already ten times higher. With all these adversities, for travel related to the Chinese New Year celebration, travellers from Wuhan transmitted this new coronavirus to just about every Chinese province where the first cases were recorded.
The very next day, on January the 23rd, all of Wuhan was urgently put into quarantine. A day later, fifteen more surrounding cities were shut down. The effects of quarantine measures on reducing the number of positive test results were only noticed two weeks later, but thereafter - it declined steadily. In the Hubei province, therefore, the new coronavirus also first entered the major hospitals of the capital, Wuhan, and put enormous pressure on them. It was at a time when many infected doctors were in isolation.
My Chinese colleagues recalled a series of decisions that then had to be made, procedures and bottlenecks that they simply couldn't have foreseen. First, their situation in Wuhan and Hubei province on January the 23rd was a "perfect storm." A large number of infected doctors were in isolation when the main wave of severe Wuhan patients were rushed into the hospitals. This is where China was fortunate to be such a populous country. All other provinces of China then sent, by emergency flights, a large number of doctors and nurses to each of the sixteen quarantined cities, with hundreds of artificial respirators shipped to them by the military.
So, they managed to bridge the shortage of health care staff and equipment until the infected doctors from the Hubei province recovered and were able to return to work. The first task for teams coming to Wuhan was to physically separate infected patients from uninfected patients in hospitals. Now they already had tests, so they could test all patients daily and know who was infected and who wasn't. One option was to move all patients uninfected with the virus somewhere else, and leave all those who were infected in the hospitals. But, uninfected patients also needed sophisticated hospital equipment. They couldn't transport them all to other provinces because for many it would be too risky. Alternatively, some Wuhan hospitals could be declared infected and others uninfected. But with these relocations around the city, the fear was that there would be chaos and eventually this virus would be introduced into all the hospitals.
Owing to that, a pragmatic decision was made clear to the rest of the world: in just a few days, two brand new hospitals would be built, and they were for the infected only. They'd be supplied with hundreds of respirators and intensive care units. This radical decision was one of the best, as it suppressed the further spread of the pathogen among hospital patients, which contributed very significantly to the total number of deaths.
Another "bottleneck" has become contagion suits for the doctors and nurses. They thought they had enough, but when Wuhan's doctors returned to work and the imported medical teams were still there, it was evident that there were simply never enough protective suits. Some factories were then ordered to mass produce protective clothing. In addition, it's important not only to have suits, but also to carry out sufficiently high-quality training among doctors and nurses on how to use them properly.
Having learned from the experience of the infection of entire medical teams at first, the directors of the large hospitals in Wuhan divided their staff into teams large enough to cope with entire wards. Such teams were no longer allowed to be in the hospital at the same time, nor were they permitted to socialise or to get in touch privately. Thus, it was ensured that if some of the medical staff were already ill, not everyone became ill.
Another practical problem was that doctors weren't allowed to take off those suits all day, so they couldn't deal with the emergencies. A large amount of adult diapers had to be purchased, which health professionals had to carry all day in their shifts. Another unforeseen problem is that the doctors in those suits couldn't breathe. After a few days, they would start developing very unsightly and painful rashes. It was necessary to mobilise entire teams of dermatologists to treat these rashes for their colleagues at the end of their shifts so that they could work again the next day.
In addition, Wuhan's hospitals were already so overcrowded with patients and doctors that it was necessary to double or triple the production and supply of food and drink for all of these people. Furthermore, the doctors had to watch over patients all day and night. Because of this, practical questions began to arise - does it make sense that they return to their homes at all during the epidemic? Most of them chose to stay and sleep in the hospital to protect their families from infection.
Others rented temporary apartments near the hospital so that they could sleep properly and not endanger their families. The third sent their families to relatives. I believe that my colleagues in Croatia, many of them my former students, are thinking about these issues now, so I'd like to offer them some ideas from Wuhan.
Finally, after suppressing coronavirus hospital outbreaks in this way, the out-of-hospital epidemic among the population in Wuhan needed to be suppressed. This could only be done by the mass testing of all suspected infected people. It was the flu and cold season of January and February, so many people were coughing anyway. It was necessary to see who was coughing because of the flu or a cold and who was coughing because of COVID-19. The Chinese then organised thousands of small epidemiology teams to report and go around the apartments, measure temperatures and test people.
Just as they had to move all infected patients from existing hospitals to two newly built hospitals, in the same way, all infected people with a milder form of the virus had to be put into isolation. They used stadiums and empty schools for this. A large number of infected people were thus moved into isolation and monitored until they were better and no longer showed any trace of the virus. So, between January the 23rd and March the 7th, Wuhan was able to completely suppress the massive coronavirus epidemic, which peaked at about 3750 confirmed infections in a single day, in just six weeks. An analogy of this for Croatia would be 1364 newly confirmed cases per day for comparison. And they were able to quarantine it within six weeks.
Lastly, I asked them how they managed to keep eleven million people in their homes so successfully. My colleagues told me that when they closed down Wuhan, the government brought together leading Chinese judicial experts.
As early as February the 6th, two weeks after the Wuhan shutdown, they enacted a "Criminal Justice Punishment Act aimed at preventing the spread of a new coronavirus that causes pneumonia." Any person who had been quarantined and intentionally violated that would be punished with "between 10 years' imprisonment and the death penalty," depending on the consequences, according to Articles 114 and 115 of the Chinese Penal Code.
If they breached the quarantine provision by accident, he would be imprisoned for a month to three years. And anyone who by any means, negligently and contrary to the instructions of the coronavirus prevention staff, contributed to the spread of the virus, would be punished with 3 to 7 years in prison. Obviously, these are penalties that were compelling enough to allow eleven million people to be kept in strict quarantine. Only one household member, every three days, was allowed to go out to get groceries for the others. Before going out, he had to call one of those small epidemiology teams to get his temperature measured.
The Wuhan/Hubei quarantine were the first mega-quarantine experiments in human history, locking 56 million people inside their households. This has shown us that the COVID-19 epidemic can be effectively suppressed. All over China, with its one billion and four hundred million inhabitants, only about twenty new cases a day have been being recorded. Most of these new cases are now coming from overseas, and the total number of deaths in China shouldn't exceed 5,000.
If the epidemic returns again with a smaller focal point, there's no doubt that China will be able to extinguish such a focal point, after such an experience. Two very difficult questions for all Western leaders today are: can they achieve the same result, and do they want to achieve it? Because months of quarantine of a lesser severity than China's will severely hurt their economies. It will leave countless people jobless.
In addition, flu caused by the influenza virus can take up to 650,000 lives worldwide annually, although vaccines are available for it. But there is almost no public awareness or fear about the threat of the flu. Perhaps a better example is pneumonia in poor children across the world, mainly caused by pneumococcus, type B hemophilus, respiratory syncytial virus and the influenza virus.
They continue to take one million children's lives per year. This is 2,739 deaths of the world's poor children every day, completely invisible and unknown to the public, due to the same medical cause that COVID-19 is now threatening us with. The West is now deciding whether to suppress COVID-19 with discipline and strict quarantine, like the Chinese, or turn it into a "creeping epidemic", so that they live in milder quarantines for months until people just get used to COVID-19 and stop it having so much of an effect.''
This text was written by Igor Rudan and translated by Lauren Simmonds
For rolling information and updates in English on coronavirus in Croatia, as well as other lengthy articles written by Croatian epidemiologist Igor Rudan, follow our dedicated section.
Croatian Scientist Igor Rudan Provides COVID-19 Quarantine Clarity
March the 12th, 2020 - If you've been following us since the COVID-19 outbreak began, we've been translating and transmitting the musings of prominent and highly cited Croatian scientist Igor Rudan. Rudan is an extremely highly educated individual who has a vast knowledge of coronaviruses.
We bring you his latest statement, posted on Facebook, translated into English in full below:
''I was pleased to see today that my namesake, Igor Stagljar, has decided to stop making press statements about COVID-19, given the psychosis we're currently in. It's interesting that a leading world scientist in Toronto, such as Igor Stagljar, doesn't feel specialised enough to write about this topic. It's worth thinking about it a bit.
Yesterday, however, I received more than thirty requests for interviews from all over former Yugoslavia, because the article in Index.hr, regardless of its extreme length, has gone viral from Kranjska Gora to Gevgelija in the past 48 hours. It now has over 6,400 Facebook shares and is crawling slightly towards 200,000 views. Respect, Matija Babic, for giving it that level of exposure.
Let's think about this for a moment too: people across the former state [ex Yugoslavia] are being educated voluntarily and massively about something scientific. I'm pleased with this, of course, so I have nothing more to add through any interviews. If I have anything new to convey that could help and save people's lives, I'll write it here, so feel free to continue sharing it further.
Your reaction to my post yesterday "Panic, but in a moral way" and the messages I got in my inbox convinced me that there are still enough people in Croatia for whom it's worth clarifying things occasionally, so thank you all. Admittedly, I will no longer be able to be regular with these posts anymore, I'm back at work. Among other things, I'm editing the current issue of the Journal of Global Health on COVID-19. A dozen excellent new scientific papers have arrived, more than half of them from China, so I'm preparing a pandemic conference for the international press here in Edinburgh in one week or so.
For Croatia, I will occasionally comment on details that few people can intuitively understand unless they've specialised in this field. The role of the occasional event commentator isn't a problem for me. Moreover, I have agreed with Drazen Klaric to continue to do so from now on for my "mother ship'' - Vecernji list, which always has the right of priority for me because it taught me to read. I managed to come to terms with Drazen about conditions that aren't too stressful for me, so I will only write for one Croatian medium, and a day later I will share those posts here on Facebook.
Now let's raise the level from which we look at everything that is going on, to show you how depressing most of the discussions currently are in Croatia, and especially the division into the camps "this is a new plague" and "this is just a flu". I called this post "contrast is the mother of clarity." It will try to explain the issues that are VERY relevant to those in power who must make unprecedented political decisions in the next 48 hours.
Many wonder how I can be so laid back when I write and talk about this pandemic. But it's like someone who professionally demining minefields marvels leisurely as he strolls through them. He knows a bit about demining, while you, walking alone through a minefield, will think that every second is going to be your last. A similar thing is happening here now.
An epidemiologist is not afraid of an epidemic because he knows that any epidemic can be effectively suppressed, it's only a matter of drastic measures. That's what I said in my initial press statements - if the situation gets worse, we have at least a few more safety nets that we can activate. Today I will explain what I meant by that, because the time has come for that.
So, if it wanted to, Croatia could become the "world champion" in the fight against COVID-19. In less than two months, we could declare Croatia a coronavirus-free zone. The total number of cases would probably not exceed 1,000, and the death toll would indeed be very small. And that's why all the debate about the severity of COVID-19 symptoms and the flu has been aroused, because that's not what an epidemiologist primarily cares about. It is important for the epidemiologist to curb the epidemic. Any epidemic will be on a safe path towards extinction when every infected person infects on average less than one healthy person. Also, it will be on the safe path of exponential spread when every infected person infects, on average, MORE than one healthy person.
Without anti-epidemic measures, this new coronavirus spreads from every infected person to at least 2.2 new healthy subjects, predominantly in the incubation phase, while the infected person doesn't yet show any symptoms. All one has to do is reduce that number to below 1.0 and the epidemic will slowly be extinguished, which can be achieved by strict quarantine.
Read that again, because that's the key thing for epidemiologists. Otherwise, it could be said that rabies is "much more dangerous than the flu" because 100 percent of those infected with it die, and in a much worse way. But for the epidemiologist, it doesn't matter, because the last indigenous rabies case in Croatia was probably recorded in 1964. And for all hunters who are bitten by a rabid boar, fox or dog, immunoprophylaxis can be easily performed, so the epidemiologist knows what to do. So, it's already starting to go that way with coronavirus. We now know that we can suppress it with strict quarantine.
For an epidemiologist, more dangerous is the disease from which more people will die this year, no matter what symptoms they have before they die, they're not so concerned with that. And if we really want to, we can suppress and control coronavirus through strict quarantines, as the Chinese did for one sixth of the world's population, with fewer than 3,200 deaths currently per one billion and four hundred million people.
So, if Croatia were to decide today that it wanted to be the "world champion" in the fight against coronaviruses, it would have to apply the following measures to prevent the spread of the virus - we'll call it "extreme left and planned" measures. It should:
- completely close and control all borders, preventing anyone from entering and exiting;
- all Croatian citizens wishing to return to Croatia should be received but be quarantined for at least 30 days before being released to their homes (this is the longest incubation recorded);
- order everyone to stay in their houses and flats for the next two months (during which time all infected people would become ill and infect other people, until the virus no longer had anyone to transfer to and would thus disappear);
- only self-service shops and an absolute minimum of public services (heating plants, power plants, telecommunications, TV and radio) would operate;
- allow only the youngest member of the household to go to the self-service once every three days (the youngest, because children have the lowest risk of dying), wearing a mask and gloves, and only if they have no symptoms;
- arrange a neighbour to go and pick up things for all elderly people and then supply that person with a mask and gloves;
- almost all patients would be treated by mobile medical teams coming to households with portable respirators; efforts should be made at all costs to avoid bringing infected persons to hospitals, so as not to cause hospital outbreaks, which would have a much higher rate of death than community outbreaks;
- banks, mobile operators, and others should be instructed not to charge loan installments during those two months.
Here, with such radical measures and completely impermeable borders, Croatia would get rid of coronavirus probably within two months, given the current situation, with a truly minimal number of deaths. It's absolutely crucial to prevent the introduction of coronaviruses into non-infectious wards. This was the main cause of the horrific numbers [of those dying] from the outbreak of the epidemics in Wuhan and Lombardy.
However, like any interesting story, this one has its own unexpected twist. The consequences of such drastic measures for the national economy would be catastrophic. Two lost months of work, to become virus free before anything else, sometime in mid-May. Just in time for the tourist season. But the problem is that others would not have succeeded by then. That is why we'd still not be able to welcome anyone to Croatia. And so, the agony for the economy would continue all summer long.
And because of the catastrophe for the economy, the number of unemployed and illiquid people will increase, people will turn to alcoholism, be depressed, suffer from insomnia, marriages will fall apart, cancer and cardiovascular mortality rates will rise. Finally, those rescued from coronaviruses will suffer from diseases that will result from a new wave of poverty and recession. Only, these diseases and deaths will not happen in front of the cameras and nobody will blame those in power for them. And for literally every single coronavirus death - they will.
If you've followed all this by now, you'll understand that in this scenario, both outcomes are, in fact, bad. But by curbing the epidemic, government officials will appear more competent, and no one will later blame them for perhaps more deaths and problems that will later arise as a result of a recession.
Another extreme approach could be called "extremely neoliberal". At the moment, Donald Trump may be intensely thinking about it, but probably at least some other countries have it. Specifically, the virus can be allowed to spread freely. In doing so, as few people would be tested for the virus to minimise the number of deaths attributable to the coronavirus, especially among very old people. It would come to, perhaps, to a death rate of up to 1 percent among all those infected, but it would save the economy and avoid that "subsequent wave" of deaths. Because in this extreme scenario, mostly older people would die. This would, from some radically neoliberal point of view, even "unburden" pension funds and the health system. Many people in the most productive age for society, who would otherwise be the majority victims of the recession, would be saved.
The problem with this approach, however, is that there should be accuracy in estimating how many people will die, that is, to gamble with the certainty that scientists have in the rate of death from a virus in the community. I estimate that it is 0.5 to 1 percent, which puts it just outside the margins around which such an approach can be considered, and that the death toll from the epidemic roughly corresponds to the estimated number of post-recession deaths.
It's possible that Trump is currently awaiting reports from American soil about these death rates and wants to have as much security in them as possible. This is like a chess game with China for him. But he came across an unforeseen obstacle, which is that with this strain of the virus in Italy, it seems like something is wrong. Perhaps that's why Trump ordered the suspension of Europeans' entry into the US today, with the exception of the British.
He may have a plan that makes him look smarter than anyone, but he knows he needs to be sure that "their" virus in the US kills less than 1 percent of those infected, with the potential to gamble on the possibility of the virus disappearing in late spring. But it bothers him, like all of us, that no one is sure of the death rate for this ''Italian'' virus. So, things are a bit more complicated than most Croatian experts on Facebook think.
Trump's biggest problem, however, is the media and the public reaction. And the worst possible choice is to hesitate between these two extremes, so deciding to "not act" and letting the virus spread greatly, but when people start to die, under pressure from the public and the media, the introduction of quarantine is too late. Because, then, it would be a disaster for both the economy and for public health. A lot of people would die and the quarantines would last much longer after such a decision, until the virus disappeared.
I've already estimated for Croatia that the "extreme left and planned" approach would immediately and now be able to stem the epidemic in our country, maybe only up to a thousand cases and with a small number of deaths, if everything went perfectly according to plan - this is the ideal, "best case scenario'' for Croatia. However, over time, several thousand people would later die indirectly as a result of the economic recession. They would probably be middle-aged and older, and would be saved from coronavirus by perhaps the same number of average elderly people. The economy would be put into reverse, but the media would rate the moves of those in power favourably.
On the other hand, the "extreme neoliberal" approach of allowing the virus to freely spread would be met with strong condemnation by the media and the public in Croatia. Thousands of people could die from the epidemic, but life would go on. Instead of about 60,000 deaths in 2020, Croatia would have about 70,000 deaths. But only on condition that we've accurately estimated the death rate of the virus and that nothing goes unforeseen.
The decision of Croatia's ruling bodies, but also those of other countries, will be somewhere between these two extreme approaches - rigorous quarantine and a complete failure to act. I think this second extreme is becoming an increasingly unlikely choice because of such an intense media focus on the pandemic. This is why many European countries are now looking at each other and waiting for what and when to do it, because it's not an easy decision.
I hope that you now understand what the current issues are which are important to people who have to make decisions over the next two or three days that will determine the lives of all of us over the coming months. Two scenarios, thirty hours. Like in a movie.''
This text was written by Igor Rudan and translated by Lauren Simmonds
For rolling information and updates in English on coronavirus in Croatia, as well as other lengthy articles written by Croatian epidemiologist Igor Rudan, follow our dedicated section.
Croatian Scientist Igor Rudan: 20 Key COVID-19 Questions and Answers
As Index writes on the 9th of March, 2020, prominent Croatian scientist and epidemiologist Igor Rudan, wrote a comprehensive text for Index in which he answered twenty key questions about coronavirus (COVID-19). Croatian scientist Igor Rudan is a member of the Royal Society of Edinburgh and the founder of the 21st Century School.
Here are twenty questions and answers on coronavirus from a highly respected and cited Croatian scientist. We have translated and transmitted Igor Rudan's text for Index in full:
''In this text, I've summarised the issues that I see most often lead to misunderstandings or cause some confusion about the new COVID-19 pandemic. I've offered all of these answers from the perspective of a scientist who has been involved in this field internationally for two decades. My answers seek to offer a view that is scientifically based on the data which is currently available about this pandemic, as well as the experience of previous epidemics and pandemics caused by respiratory viruses.
However, I'd like to emphasise the fact that there is still a number of ambiguities regarding the new COVID-19 pandemic and that scientists are closely monitoring its development and gathering new evidence, which is why this pandemic needs to be taken seriously and adhered to by all public health experts. In the event of this situation worsening, one should also be prepared for preventive public health measures such as avoiding public gatherings and quarantines at home.
1. Is this one of "those" infectious diseases that will decimate us and which will take its place in history?
The history of the genus ''Homo'' and the dozen human species we know of today through excavation was determined by the fight against infectious diseases. It's likely that the species that are no longer around today are largely extinct due to the spread of infectious diseases. We should be happy that we no longer live in the times of great epidemics and pandemics that once decimated our species. A huge number of people died during their childhood or youth.
The most severe medieval infections killed up to every third person, and before the discovery of the microscope, people couldn't even know why it was happening to them. No one thought that tiny, invisible, living microbes could cause these diseases. People assumed that some heavenly punishment for their sins had come upon them. We should, therefore, be happy because we're living in the age of this advancement of science and medicine.
Since 1940, many bacterial diseases have begun to be controlled by antibiotics, and since 1960, many virus and bacterial diseases have had vaccines developed for them. Unfortunately, we don't have a vaccine for all infectious diseases. As we see in the example of this pandemic, new viruses continue to transfer over from other species to us because history hasn't ended with the advent of our generation but instead it just continues.
2. Could science have expected the COVID-19 pandemic?
It could have, because this is already the seventh coronavirus to try to make itself at home within the human population, trying to adapt to us and use us as its reservoir. Specifically, we exist together on a small blue-brown planet in a vast dark universe. We share it with tens of millions of other species. They all strive to survive until further notice. More than 99 percent of all species that have ever existed on Earth have failed to survive to this day. That is why viruses must constantly transfer themselves to new species and thus expand their reservoirs. They must choose the winning species because they can't reproduce on their own. Their survival depends on the survival of the species that is their reservoir.
People are currently an interesting potential viral reservoir. We're expanding and multiplying rapidly - from about a billion and a half individuals, we've grown to about seven and a half billion in the last 130 years alone. In doing so, we're penetrating territories, clearing forests, draining wetlands, hunting for pleasure, reducing overall biodiversity, making it difficult for others to survive, while there are more and more of us. Fortunately for all of us, the first four human-adapted coronaviruses were merely the cause of common colds. No one considered them a serious threat to public health.
3. Were SARS and MERS a serious threat?
SARS (severe acute respiratory syndrome) and MERS (Middle Eastern acute respiratory syndrome) were a real and big surprise for scientists and experts. Specifically, these were respiratory viruses from the coronavirus family, the fifth and sixth that were able to pass over to humans. Surprisingly, instead of colds, they could have caused very severe, fatal pneumonia. In addition, the death rate among those infected with both diseases was truly frightening. Both could have caused a horrible amount of death of humans if, by chance, it had spread to the world's entire population.
The coronavirus that caused SARS had its reservoir in bats, which hibernate in caves in winter. Then, no one hunts or consumes them. However, it did manage to transfer over to an animal from the cat family, a civet. It was also contracted by a man, a farmer in Guangdong province, in late 2002, from a civet. SARS then spread to more than twenty countries and infected more than 8,000 people, with every tenth person confirmed to be infected. It was the fifth human coronavirus, but it was the first to kill humans.
Ten years later, in 2012, the MERS coronavirus appeared in Saudi Arabia. It was passed on to humans from the camels in the desert. It has also spread to more than twenty countries, infecting about 2500 people and every third infected person died. So, MERS had a really scary mortality rate. The advent of MERS showed us that SARS was not some isolated incident with a coronavirus that we can just forget, but that coronaviruses have become our most significant potential enemy. If SARS or MERS had spread around the world and infected billions of people, it would have been a catastrophe unlike anything from the last century or two, that is, in popular culture, it would've been called the "zombie apocalypse."
4. How did MERS and SARS manage to be dealt with so quickly considering the fact that they were so dangerous?
In those two cases, we were actually very lucky. Namely, a completely new virus that tries to transfer over to the human species can spread in humans in three basic ways. These ways depend on our ability to deal with epidemic surveillance. Once the virus enters the human body, it begins to multiply in the kind of specialised cells that it has been able to bind to. In the case of coronaviruses, these are the cells of the respiratory system. It multiplies in them by "hacking" its cellular genetic instruction and using that "machinery" to build proteins.
This multiplication of the virus destroys the cells, which is why there are symptoms characteristic of problems with the respiratory system: such as a sore throat and cough. In the first mode of the spread, the virus spreads from the infected person to other people only after the onset of symptoms.
It is easiest to stop such an epidemic because the sick person no longer leaves home. Therefore, it mainly infects only their household members. It's also relatively easy to identify who was in contact with the person after the onset of symptoms and also put those people in isolation. We were fortunate that both SARS and MERS spread to other people only after the onset of the symptoms of the disease, so we were able to suppress the epidemics by isolating those infected and all their contacts after the onset of the symptoms. This is the most important reason why SARS and MERS didn't manage to kill an incredible number of people.
It's much more difficult to stop an epidemic if the virus spreads from the infected to the healthy during the period of the so-called incubation, which lasts from the entry of the virus into the body until the onset of the first symptoms. Then, the infected person can transmit the virus by contact to a significantly larger number of people in the days before they get any symptoms. That's the situation with this new COVID-19 pandemic. But even then, it's at least possible for every new patient to determine from whom he or she has previously contracted the infection. Namely, they had to meet somewhere, so it's possible to follow the whole chain of movement of the virus from person to person.
Due to this, intensive isolation measures of all those exposed to those already infected can significantly slow down the spread of the virus. This was done in Wuhan. That's why quarantines are justified and that's why they give good results.
A nightmare for any epidemiologist, however, is a third possibility for the virus to spread. In such a variant, people become infected and transmit the virus, but they themselves never show any symptoms. Scientists are currently looking for such possible spreads of contagion with this new COVID-19 pandemic. That's why such persons are occasionally mentioned in the media.
Namely, because of such infected people, cases are beginning to emerge among the population that can't be linked to any of the already infected people. When people are circulating in the population without symptoms but passing the virus on to others, it's very difficult for epidemiologists to do anything to prevent it from spreading among humans. Such an epidemic has the potential to spread over time, mainly due to such transmitters or carriers who show no symptoms.
5. What makes the new COVID-19 outbreak different from the previous six coronaviruses?
When something has happened six times in a system as complex as the Earth's ecosystem, then it's no surprise that it's happened for the seventh time. Another coronavirus is trying to make itself at home now in the human species. In this case, the primary reservoirs were probably bats again, because the genetic sequence of this new coronavirus coincides with that found in hibernating bats in about 96 percent. This time, instead of a civet, a smaller mammal or bird has served as coronavirus' transitional reservoir.
It's possible that it was a shellfish, because in one of them, a coronavirus that matched to the human form in as much as 99 percent of the sequence was found, although this isn't completely definite either. Sequence matching is not the only important factor when it comes to transfering to humans. What's also important is how many individuals in the species that serve as the transient reservoir are infected and how often the species comes into contact with humans. Sometimes these factors are more important, so they can bridge the gap of 2 percent or 3 percent of the genome difference, because bats are a protected species and can't be eaten.
Thus, in the Chinese province of Hubei, in the City of Wuhan, which has a population of eleven million, at around the end of 2019, the number of patients with unusual and very dangerous type of pneumonia began to increase around the fish market. It was soon discovered that this disease was spreading very quickly. Each infected person managed to successfully further infect as many as two to three people. Such a degree of infectivity is very high and leads to rapid growth of the epidemic. We had the misfortune of COVID-19 apparently managing to spread even during the incubation period, probably by touch.
This incubation period lasts about five days on average, and it becomes very tricky when it lasts longer. However, an incubation period of up to two weeks isn't that unusual, and incubation cases of up to four weeks seem to occur. During all this time, the infected person may spread the virus before the onset of any symptoms. If there are also infected people who don't develop symptoms, it will be extremely difficult to completely reverse this pandemic until we develop a vaccine for it. In conclusion, infectivity, ie, the ability to move from the infected to the uninfected, was significantly higher in COVID-19 than it was with SARS and MERS. But that's why we now know for sure that the COVID-19 mortality rate is still significantly lower than that of SARS and MERS.
6. What is the death rate among those infected with the COVID-19 epidemic, and why is there so much ambiguity about it in the media?
First, I will clarify that in this text, for ease of reference, I use the term "death rate" instead of the term "lethality" or "case-fatality rate" and to distinguish it from the term "mortality rate", which would refer to the term "mortality". In order to answer this rather complicated question, it must first be said that nowadays, the registered number of infected persons and the number of deaths can be monitored online.
When the registered number of infected people was divided by the number of deaths at the beginning of the pandemic, a figure of about 2 percent would be obtained. From this, one could apparently conclude that this coronavirus is new and so nobody is immune to it, which means that it will spread throughout the world over time and infect us all. If it kills 2 percent of all people, then it's not hard to calculate that out of 7.5 billion people, about 150 million will die from it. And it's difficult for anyone who is not a specialist in this field to understand how such an outcome can now be prevented at all, because a vaccine against this virus doesn't yet exist, nor do medicines.
The question of the death rate among those infected with COVID-19 indicated a general misunderstanding of the epidemiology profession in the public and in the media. From the very beginning of this pandemic, there were people who claimed that the new coronavirus was a disease milder than even the flu, but also those who believed it was significantly more dangerous. In recent days, this issue has finally caught the attention of all the world's media as the World Health Organisation reported "that about 3.4 percent of those infected with coronavirus have died." That sounded terrifying to the media and the public.
But then US President Donald Trump also made a public statement saying the number released by the WHO was "wrong." He said he'd talked to people who knew something about it and that his impression was that the number was certainly below 1 percent, if not significantly less. In my guest appearance on Sunday at 2 (Croatian TV show), I made my estimate of the death rate of 0.5 to 1 percent, with the possibility that it would be smaller.
However, both Trump and WHO are actually right, each in their own way, which shows best and how difficult it is for many people to keep track of what is really going on because of their ignorance of this profession.
In the beginnings of every viral epidemic, the virus still has to transfer over to humans, and that can be difficult. Therefore, they will choose those with a weakened immune system, who will have a harder time rejecting it. Because of this, the first patients are often people who are either older or already have some underlying illnesses that make them more vulnerable. They end up in a hospital, where at that point no one doubts the epidemic potential of their pneumonia.
They then become infected by other hospital patients, and by some healthcare professionals. The latter then spread the disease to other patients in the hospital - very sensitive people, the elderly, patients being treated for serious illnesses. For this reason, the proportion of deaths among all COVID-19 patients was initially very high. That's how it started out in Wuhan, and in exactly the same way in Italy - they died of infections in hospitals, and they were mostly very old and sick people.
In the meantime, the virus has started to spread among the general population, those outside of hospital situations. It has infected many people who are otherwise healthy and has as such better adapted. A large number of these people thought they had a cold, or the flu, and maybe even a more severe flu, which they were just letting run its course, resting at home. Considering that it was flu season in Wuhan at the time of the outbreak, and it was reported that something strange was happening in hospitals and that people were dying on a larger scale, it is now understood that many with the coronavirus stayed home and treated themselves.
Few people wanted to go to the hospital to have tests for the flu because of coronavirus, when a seemingly very deadly epidemic was brewing there. Only the few who have struggled with fevers and symptoms for more than eight or nine days sought help from Wuhan hospitals.
In China, there is typically no primary health care and family medicine as we know it, but there are huge hospitals in their huge cities where patients report directly. That's why the death rate among patients at Wuhan hospitals at the beginning of the epidemic was so frighteningly high.
7. Is the infection of the most vulnerable in Wuhan hospitals early on in the epidemic the sole reason for the high initial death rate of COVID-19?
It isn't. The epidemic seemed even more dangerous at first, as it created a great deal of pressure on hospital intensive care units, which were unprepared for this infection. As a result, all severely ill patients could not receive intensive care. This further increased the mortality rate at the beginning of the epidemic. That's why the Chinese have started building new hospitals - to have sufficient capacities to be able to provide intensive care and to move all those infected with COVID-19 away from other seriously ill people who are sick because of other diseases, who are at the highest risk of dying if they do become infected.
Based on this, it should be understood that the total number of those infected with COVID-19 in Wuhan was much higher than what was confirmed by health statistics. Specifically, only those with coronaviruses who were eventually admitted to the hospital were confirmed to be infected and were tested for the new virus there. They are by no means representative of all those infected with the new coronavirus in Wuhan.
Their mortality rates cannot, therefore, be mapped even in terms of the population of the total number of those infected with coronavirus in Wuhan, let alone the entire population of Wuhan - ie, all infected and uninfected people. Therefore, it's completely wrong to look at the number of confirmed infected and the number of deaths on the Internet and divide the number of deaths by the number of confirmed infected people and draw any conclusions from that.
8. Why does the number of infected and deceased people on the Internet, which is constantly being updated, give a wrong impression about the death rate of COVID-19?
If the deaths are divided by the confirmed number of infected people, then both the numerator and the denominator are completely wrong when it comes to calculating the actual death rate. Even deaths in the numerator are wrong because if we monitor the confirmed infected and those who have died in real time, that is, day by day, it can be understood that a great many infected people haven't even had a chance to either recover or die.
People in intensive care will die for days, weeks, maybe months, which is why the death toll in numbers will increase over time. In doing that, some future number of registered deaths, as the numerator, will increasingly correspond to the current number of registered infected persons, as the denominator. The mortality rate of "deaths through confirmed infection" will then no longer be 2 percent or 3 percent, but may increase over time, perhaps to 6 percent or 7 percent.
Therefore, to say that "3 percent or 4 percent of those confirmed to have been infected so far have died" isn't really wrong in itself, which is what the World Health Organisation did. But what it missed is explaining that this mortality rate among confirmed infected people is quite unrepresentative of the mortality rate among those infected, which is much lower. It wouldn't surprise me, as an epidemiologist, if it is up to ten times smaller, maybe more. This could ultimately make COVID-19 a less deadly and dangerous disease even than the common flu.
9. Can you be sure that the total number of infected people is much higher than the number of registered infected people, is there any evidence for this?
Given that the virus is new and unknown, this is a key question. Unfortunately, the possibility that this virus is quite different from known ones must also be allowed. It may be that the rate of deaths among confirmed infected people is only 3 to 5 times lower than the death rate among the number of all infected people, and not ten or thirty times lower. The only sure thing is that the number of confirmed infected people certainly didn't quite equal the number of infected in Wuhan. The current global totals for COVID-19 are still largely determined by what happened in Wuhan at the beginning of the epidemic, since about two-thirds of cases worldwide still originate in Wuhan to this day.
That's why I've already explained on Sunday at 2 that the mortality rate among confirmed infected people is not so important to us because it's a subset of the most severe patients. You should know the mortality rate among the total infected people. However, no one can know that at this time, because at least 100,000 Wuhan residents would need to be tested for this and then the presence of antibodies against coronaviruses should be detected.
Accordingly, we'd also know the proportion of people who got over it without ever even seeing a doctor. So far, no one has conducted these studies because the health system was preoccupied with the diagnosis of coronavirus in hospitals and even struggled with it. It's now known that during some days of the outbreak, while it was spreading, there were not enough tests for all those who had symptoms.
However, the first additional evidence is beginning to emerge. The first is the report of an international panel of experts who visited China. They concluded that when looking at just about all cases across China that were reported after February the 1st, when the identification of all those infected was significantly improved, and hospitals were better prepared for the epidemic, the mortality rate of all cases that came under health surveillance and were tested dropped to 0.7 percent.
For all those skeptical of China's data, we've also received reports from South Korea. In that country, the authorities have really done their best to aggressively test people, seek out all those infected and isolate them and treat them. In their analyses to date, the death rate of all infected people has been slightly above 0.6 percent. Both of these figures could increase slightly, but not really significantly, if they also included those who could die over time, and are currently counted as infected, but at such a low rate of death, there won't be as many. It's more likely that many infected people remain undiagnosed and the rate is actually even lower.
Another interesting recent new source is the study of more than 1000 COVID-19 patients followed up right up until the end of the infection, collected from over 500 Chinese hospitals, published in a top scientific journal. It showed their mortality rate of 1.4 perent. However, it was not all those infected again, but those who requested hospital treatment, and therefore it should still be at least two to three times less among all those infected.
Thus, it appears that data from very different and increasingly reliable sources are starting to converge to the values I predicted on Sunday at 2 a week ago, i.e. 0.5 percent to 1 percent. Because of all of the above, US President Donald Trump is most likely right to say that number is certainly less than 1 percent, and he believes it could be well below 1 percent. Everything we know about epidemiology and previous pandemics gives us hope that this could be the case.
10. Can anyone in a country be infected with a coronavirus? If so, would the death rate of 0.5 percent or 1 percent be applicable to the whole population then?
The virus will not succeed in infecting just about everyone in Croatia for a variety of reasons. The front line of defense is currently anti-epidemic measures. All those who may be infected are being tested, and then COVID-19 patients and all their contacts are isolated.
These measures significantly slow down and prevent the spread of the virus in Croatia and buy us some time. It's of utmost importance that the number of patients doesn't increase too quickly, in order to enable the staff of our health care system to provide quality care to all patients, and if necessary - intensive care. In the absence of these measures, there would be an exponential increase in the number of infected people, which would soon become intolerable for the health system. We're also protected by our geographical dispersion, ie, there are many people living in smaller towns and settlements. A large number of them will probably never be entered by an infected person.
Furthermore, as people become infected and get over it, they should become immune to the virus. As a result, there will be fewer and fewer people the virus can transfer to. At some point, the number of new people that infected people can spread coronavirus to will decrease to an average of less than one. This will limit and stop the epidemic itself. That's the reason we vaccinate - to disable the virus, even if it infects some unvaccinated people, it has less options for further spread. Specifically, some people will already be immune to the virus and their bodies will reject it if the virus tries to get into them. Many processes in nature are self-limiting in a similar way - forest fires and epidemics.
Furthermore, in the Sunday at 2 broadcast, I also explained why the finally determined death rate among all those infected should not be directly mapped to the entire population of a country, in order to estimate the possible death toll. The first reason is that the virus mainly affects the elderly. That's why this established rate of death among all those infected can be projected only on the elderly, but not on young people and children. Young people and children rarely get sick and their death rates are much, much lower. This further contributes to the diminishing potential of the virus to cause a very high number of COVID-19 casualties.
11. Should we then fear the COVID-19 pandemic, and if so, how much?
The situation should be taken seriously and people should be cautious, but there's no reason to be overly afraid, there's especially no reason to panic. I understand that many people are afraid of this pandemic because they probably think we're in a completely unfamiliar situation, so anything could happen. But it's unlikely that much could happen for which science could not find explanations and answers, and the epidemiological services responded in a timely manner. Although it's not good for a serious scientist to try to predict anything about the spread of a completely new and unknown virus to the entire human population in the world and to predict each individual event, we have in recent weeks collected enough information about the new COVID-19 virus for at least some predictions.
If the new coronavirus completely spreads across Croatia over time and manages to circumvent the many prevention measures currently in place, its casualties should be at least roughly comparable to the deaths from flu or road accidents in the same period. This means that some healthy caution is advisable. This caution is reasonable as long as it is on the same level as the fear you may feel when sitting in a car and preparing for a longer trip, or when you hear on the news that a more severe form of influenza has arrived in Croatia.
But many wonder why coronavirus is written so much about and why it attracts such a level of attention. This is because flu has been a well-known disease for decades, it comes back every year and we have experience with its manifestation in tens of millions of patients worldwide, we know how to develop vaccines against it in advance, and we've started to get the first somewhat effective drugs on the market. Unlike the flu, the new coronavirus is unknown to us and we're most cautious about not being unpleasantly surprised. At the same time, the most vulnerable among us, who are already seriously ill or very old, aren't vaccinated, as is the case with the flu, so this new disease can kill more easily.
12. Is it now quite clear that COVID-19 is a significantly more dangerous virus than the flu?
This question has constantly been being raised since the beginning because many are looking at various figures without a deeper understanding of their background and are comparing the incomparable.
First of all, the general public underestimates how dangerous and serious the flu actually is, especially for the most vulnerable, the elderly and the already ill. In the world, influenza causes between 250,000 and 650,000 deaths annually, depending on the strain of the circulating virus. Different strains can cause milder or more severe symptoms, and the virus mutates year after year. However, we try to prepare those most vulnerable before the flu season begins.
Therefore, the number of deaths from influenza is reduced by preventive health intervention, ie, vaccination, and this can't be done with the spread of COVID-19. This is the first reason why the flu seems less dangerous, but it may be no less dangerous, it's just that we protect the most vulnerable. In addition, flu vaccinations make it more difficult for it to spread among the population because there are fewer options for it to transfer to the uninfected. Due to the slower spread, new cases are slower to emerge and the health care system has time to deal with them properly, especially if they require intensive care.
Another reason is that the number of deaths directly from the flu is several times lower than the number of deaths indirectly from the flu. Influenza is often not cited as a direct cause in statistics on the causes of death, if it has merely led to the exacerbation of some of the long-present chronic, underlying disease. These chronic diseases are then cited as the primary cause of death, and not influenza. Therefore, the actual role of influenza in total annual mortality is often significantly underestimated. It could also be several times higher if the cause of death were reclassified at the end of each year, given the increase in deaths from chronic diseases during the flu season.
The third reason is that we have a much better idea of the total number of people truly infected with the flu than we do with coronavirus. This is because influenza is a disease that is typically managed around the world within primary care, after which patients are referred to home care and only the most serious cases end up in hospital.
Due to the obligation to report to the central registry, as well as for sick leave, the total number of people infected with influenza in the population, ie, the denominator for death rates, is much better known to us than the coronavirus. COVID-19 has so far been diagnosed and treated exclusively in hospitals for severe cases. Their estimates of death rates include patients suffering from ''hospital outbreaks'', which have spread to the elderly, the sick and the immunocompromised.
From all of this, it should be concluded that the rates of death from influenza, as a very dangerous viral disease, have been mathematically reduced compared to the current reports of death rates for coronaviruses for the three reasons I mentioned. The first is to vaccinate those most vulnerable to the flu before the flu arrives. Another reason is that health statistics don't record the majority of flu deaths as deaths from influenza, but because of the exacerbation of pre-existing underlying illnesses such as cardiovascular disease, diabetes, malignant tumors and other things.
The third is that the denominator we use to calculate the death rates from influenza is much closer to the total population actually infected, while the denominator for coronaviruses is not yet known with sufficient certainty. Epidemiologists, from experience with other respiratory viruses, know that all events in hospitals that affect among the most vulnerable, should by no means be mapped and placed alongside the healthy. However, the general public who is not in the profession cannot have a good sense of this huge difference. That's why all death rates from the number of people infected with the flu are not currently comparable to all the death rates of coronaviruses currently being managed.
While the general public, on the one hand, underestimates the risk of influenza for three reasons, it is also easy to overestimate the risk of the new coronavirus due to its intense media focus. If influenza in Croatia was monitored in this way each year to report on each infected person and their influenza testing, almost every day at least one person in Croatia would die directly from the flu during the winter months, and three or four more would die indirectly. Then the public would realise how dangerous the flu really is and how reasonable it is to be vaccinated against it.
Therefore, it still doesn't seem possible to me, at least at this stage of the pandemic, to decisively state which of the two diseases is inherently more dangerous to humans or which will cause more deaths this year. Flu will, at least apparently, cause fewer deaths because the most vulnerable go for vaccinations, and many of the deaths it causes are not attributed to it in health statistics. COVID-19, in turn, will cause fewer deaths than it could due to epidemiological surveillance, the prevention of its spread and possible severe quarantine, and it may also have seasonal characteristics and simply disappear with the arrival of late spring.
13. Are such strict quarantines justified?
When we have no other means of defending ourselves against the new virus, all we can really do is retreat indoors and prevent the virus from travelling from infected to healthy individuals. People generally don't have an intuitive sense of exponential growth.
If each newly infected person infects just one more person each day, the number of newly infected people will increase from 2 to 16 during the early phase, which doesn't seem like a big increase. A little later, it will jump to 1024 infected people from 128 over the next three days, and that doesn't sound so terrible either. But there will also come four days in which the number of newly infected people will increase from 100,000 to 800,000.
When China saw that the COVID-19 epidemic was out of control and entered that explosive phase, it immediately cut off Wuhan and then fifteen other cities from the rest of the country. In addition, it ordered that the population within these cut-off areas stay in their apartments and not leave. It was an unprecedented measure in human history - tens of millions of people were quarantined for weeks. Everything stopped.
However, this measure produced excellent results and China could stop the death toll of less than 5,000, although the epidemic found it unprepared and the virus spread to just about every province. A recent report from a World Health Organisation commission made up of 25 international experts visiting China concluded the following:
"The very bold Chinese approach to preventing the rapid spread of this new respiratory virus has changed the course of a then rapidly escalating and deadly epidemic. Faced with an unknown virus, China has implemented probably the most ambitious, agile and aggressive effort to combat infectious diseases - ever. This uncompromising and rigorous non-pharmaceutical measure of ordinary quarantine in curbing the transmission of COVID-19 virus in multiple contexts is now providing us with key lessons in planning a global response.''
14. What happened on the Diamond Princess ship, which is also isolated? It appears to have a death rate of more than 1 percent for those infected. Isn't that very informative for scientists?
I can only say that this may be because, on these large ships, people are mostly older, because one should look at the age and gender structure of passengers, which, I believe, would explain at least something more. Also, it is quite possible that a mutated version of the virus, which is somewhat more dangerous, also enters into such a pocket, and such isolated groups emerge in which the disease actually ran a more severe course. This is not impossible, but it also isn't likely that it can be mapped to the entire population of a country.
The virus, now spreading through the human species, continues to mutate in order to adapt to us as quickly as possible. According to previous epidemiological experiences, many of these mutations should make it less dangerous for our health, as they will be better adapted to us in this way. However, some random mutations could make it more dangerous, and we need to be on our guard until we get better acquainted with it and the pandemic is over. It's unlikely that the new coronavirus will mutate to become significantly more dangerous than it is now, but we'll only be able to assert that for sure when the pandemic is over.
15. What's happening in Italy and Iran? Does COVID-19 behave differently there than it does in other countries? Could the development of a mutated, more dangerous variant of the virus be the reason?
These are very difficult questions to answer until we get more quality data from both countries. In principle, it's possible that the first entry of the virus into a new country may be in the body of an infected person, in which the virus has mutated into some more severe form. If all further cases come from this mutant and a more dangerous virus, then in these countries, the situation may initially seem more difficult than elsewhere, until other carriers emerge. In population genetics this development is known as the so-called "founder effect" - the effect of the founder. However, both of these countries may also have different explanations.
The reason why the rate of deaths among infected people in Italy appears to be very high is because even there, the disease spread in small-town hospitals which were completely unprepared for the epidemic, and among the elderly who are at much greater risk of dying if they become infected.
The death rates in hospital outbreaks among older, sick, and possibly immunocompromised people will be much higher than those in the community, among healthy and younger people. Among the top 100 deaths in Italy, almost all people were over 60 years of age and had underlying illnesses. That's why the mortality rate seems so high there, but it just isn't representative of the entire population. Seasonal flu would probably have done similar damage if many had not been vaccinated against it. But it's also possible that there are many more cases in the population than previously thought because the virus has been spreading for a long time. In Iran, however, the situation is unclear so far. The most likely explanation, too, is that there are already significantly more cases of infection than was imagined among the population.
16. Is it possible that coronavirus may surprise us and ultimately prove significantly more dangerous than seasonal influenza and kill more than one million people in the world, or even several million?
If COVID-19 proves to be significantly more dangerous than seasonal influenza, then one million deaths worldwide could indeed be expected, perhaps significantly more. Unfortunately, such a scenario is still possible in principle with a virus that is new and unknown to us, for a variety of reasons. Because of this, all experts in the field, including myself, are constantly urging people to take caution, but without the unnecessary panic.
In which scenarios could the situation become much more difficult? Firstly, most epidemiologists, based on their experience with previous epidemics and pandemics, expect the COVID-19 mortality rate to fall well below 1 percent when the death toll begins to be shared with a better estimate of all infected people. However, the virus is new, so it's possible in principle for this specific virus that the number of infected individuals not registered may not be as large as epidemiologists would expect. This would come as a surprise to science and would indicate a different nature of this virus.
The new coronavirus causing COVID-19 is somewhat similar to that caused by SARS. The SARS pathogen, however, had an extremely high death rate among all those infected. If the total population infected is found to be higher than the registered infected population by only two or three times, and not by at least ten times, then the death rate of those infected with COVID-19 could be significantly higher than the flu.
Combined with the lack of a vaccination, because we don't have vaccines for it, it would lead to a significantly higher number of deaths than the flu. However, such an event will be prevented by measures of isolation of the patients and their contacts, as well as by quarantines, which aren't applied to the flu. We also hope that the passage of winter and the arrival new seasons will become our allies, which will slow down or completely hinder the further spread of the virus.
Furthermore, the virus could spread to infected people in some of its more dangerous forms, as well as in milder forms. Previous experiences with epidemics have shown that mutation into milder forms is more likely, but mutation into more dangerous forms, or those that are more easily spread, isn't impossible either. In some countries, such a variant would increase the death rate locally compared to other countries or accelerate infection.
This would put their health systems in a really difficult situation as intensive care units would soon become overloaded. With poorer care available, the death rate of all those infected would increase further, with the collapse of part of the health system. It's also a very tricky scenario in which many healthcare professionals would become infected over time in providing care to patients, which would make the situation worse.
Therefore, currently, perhaps the most important citizens of Croatia are all those healthcare professionals who work in hospitals for infectious diseases, especially in their intensive care units. They should be protected from work overload but also from coronavirus infection by their patients. With the increasing number of infected people, the demand for quality intensive care, respirators and ECMO devices for extracorporeal oxygen enrichment and the doctors and nurses in these wards will become the "bottleneck" of the health care system, which should be amplified and further strengthened before they come under increased pressure.
The worst-case scenario imaginable to epidemiologists right now is the entry of some more dangerous, mutated version of coronavirus into one of the very poor countries in the world with a poor health system. Such countries cannot implement satisfactory quality epidemiological surveillance measures. Then, a more dangerous version of the virus would infect a large percentage of the country's population relatively quickly. Panic would ensue, probably also a black market for the transport of migrants to other countries. Then COVID-19 would start to expand uncontrollably and in a whole new way.
In the event of any of these unfavourable developments, which are all unfortunately possible, though not likely, we'd need a completely new protection strategy. Each country will have its own approach. When the death toll in each of the affected countries begins to rise so much as to cause fear among the population, people will become more willing to take much stricter measures. In such a case, more and more countries will resort to a "Chinese" solution that has proven effective in Wuhan - declaring large, very strict quarantines. It's essential to buy time in such quarantines so that health systems don't become overburdened and to anticipate the end of winter and the possible seasonality of this virus, which could then begin to spread in a weakened manner or disappear altogether, at least until next winter.
17. With these reasons for caution and adverse scenarios, is there any reason for possible optimism?
There are at least several reasons for optimism. First of all, epidemiological surveillance and "front lines of defense" are currently in place throughout the European Union. If it works well in most countries, it's possible that their outbreaks will be controlled and not go into a phase of exponential growth in the number of cases. In the most favourable scenario, with this retention, this coronavirus would show seasonality and slowly disappear from circulation with changes in nature characteristic of late spring and summer. However, this is the most favourable scenario, in which the final death toll would be much lower than that already caused by the flu this year.
However, if the front line of defense and epidemiological surveillance is broken through by the virus, then governments will resort to strict measures to ban assemblies and organise quarantines, as the Chinese did. Several models done in recent weeks indicate that strict quarantine should completely suppress the spread of this coronavirus within three months. This is exactly what we've already seen in China. That's why it seems to me that one great positive lesson of this pandemic is that humanity today would be able to survive even more dangerous infectious diseases than COVID-19 with strict quarantine, in which people would remain until scientists developed vaccines. This is really a new situation that has shown us this.
Finally, the tireless work of numerous scientists currently testing over a hundred drugs against this virus, as well as at least eleven experimental vaccines, should be noted. It is also impossible to get recommendations on the use of medicines in the foreseeable future, and vaccines should become available over time. In this unusual situation, these are all unknowns that could at some point become important and make a significant difference.
18. With the effectiveness of quarantine in China, can we draw any lessons from this pandemic?
We should always strive to find something good in all the bad things that are currently happening to us. I hope from this that many people will finally realise how dangerous flu is and start to get vaccinated against it. Each year, the flu kills between 250,000 and 650,000 people worldwide.
In China, which is one-sixth of the world's population, the death toll from COVID-19 could be stopped below 5000 by the Wuhan quarantine. If all other countries could implement anti-epidemic measures like China, then the death toll from COVID -19 could be at most six times higher, ie, up to 30,000. That would be ten times fewer deaths than the total number of deaths caused annually by seasonal influenza. Unfortunately, many countries will not be able to follow China's example closely and will have uncontrolled outbreaks if the warmer season doesn't stop the spread of the virus.
Furthermore, if the virus continues to spread throughout 2020, it will demonstrate in a very cruel way how well the public health systems of individual countries function. It will be possible to produce performance charts for each country in controlling this new infectious disease, given the population size and age structure. These will be very important lessons to learn in preparation for a future pandemic, which could be even more dangerous.
Additionally, the virus generally spreads by contact. This means that it's good to be reminded that hands should be regularly and properly washed during epidemics, you should avoid touching surfaces that many people touch (knobs, handrails, ATMs), avoid shaking hands, keep at least two steps away from people who have symptoms of respiratory infections, and it's also advisable to regularly ventilate your living quarters. It's also helpful to work to strengthen your personal immunity with sufficient sleep, exercise and good nutrition.
19. Are there any real surprises for science related to this pandemic, at least for now?
Very few [surprises], I'd say. I explained why it's no surprise that after the previous six coronaviruses, the seventh has now manifested in a human. Nor is its spread rate a surprise, as there are both significantly more infectious and much less infectious respiratory viruses. It would be somewhat surprising for epidemiologists if the number of the total infected people in the population wasn't significantly higher than the number of registered infected people, which would raise the death rate significantly above that of the flu. We continue to await the information of well-conducted studies on this.
Perhaps the biggest surprises are related to the clinical course of COVID-19 rather than the epidemiology itself. For now, clinicians in China have reported that registered infected people report to the hospital rather late, on average after as many as 9-12 days of home care. This may be a reflection of their fear of being admitted to the hospital during an epidemic, but it may also be an interesting feature of infections with slow development over other respiratory infections. Furthermore, fever doesn't appear to accompany other symptoms of the disease in the first few days, making it difficult to locate cases by controlling people's temperatures.
The media has also reported on the possible return of the virus after suffering from the infection in some cases. For now, it's hard to know how common these cases are, and how many exceptions there are. Many viral respiratory infections always need to be "rested", that is, to allow the body to recover for a day or two after the infection has ended, as it is unknown whether or not these infections can return if the immune system has not completely removed the virus from the body. But with all new and unknown viruses such surprises are possible, so one should be careful until the pandemic is over.
20. What are your closing messages?
In all the answers I have offered in this article, I've endeavored to convey an insight into the most likely scientific explanations for the abundant information that is published about COVID-19 in the domestic and international media. Over time, some of the likely scientific explanations may need to be modified in the light of new information. One shouldn't forget that this is a new virus, so surprises and deviations from the expected scenarios are in principle possible. That's why I emphasise that caution is needed, but not panic. I will monitor the further development of the pandemic.
Obviously, we need to prepare for a serious flu-like illness against which no one will be able to be vaccinated. Therefore, elderly people and those with underlying illnesses should be extremely careful because the infection is very dangerous to them. Having gained our first knowledge of COVID-19, we now need to concentrate on preventing the spread of the virus in Croatia and buying our time in regard to the weather until the arrival of warmer days, when we might be lucky enough to slowly stop the virus from circulating due to seasonality. Unfortunately, we can't know that right now. From everything written, it should be understood that all measures of active searching and the isolation of patients and their contacts are justified.
These also include bans on gathering together larger groups of people, as well as possible quarantine if the epidemic starts to elude control. Particularly, older people should be looked after because the probability of a bad outcome increases significantly with age. In addition, those with heart disease, diabetes, or undergoing cancer treatment should take special care.''
This text was written by Igor Rudan and translated by Lauren Simmonds
For rolling information and updates in English on coronavirus in Croatia, as well as other lengthy articles written by Croatian epidemiologist Igor Rudan, follow our dedicated section.
Croatian Professor Igor Rudan Addresses Media on Coronavirus
Igor Rudan is a Professor of International Health and Molecular Medicine at the University of Edinburgh in the United Kingdom. The Croatian professor issued a press release intended for the Croatian media and its representatives in the form of a Facebook post on his personal account.
We have transmitted and translated the post in its entirety below:
''I would like to thank everyone for the truly incredible amount of interest and calls that came to me today from virtually all of the media in the Republic of Croatia, to try to calm the atmosphere that has begun to emerge in Croatia because of the first COVID-19 coronavirus patients, as an internationally recognised expert in the field of global health.
I hope you can understand that as the director of a major global health research centre and the head of a World Health Organisation Collaborative Centre at the University of Edinburgh, United Kingdom, I've a lot of work to do over recent days and it's completely impossible for me to respond to your individual requests. Therefore, in this way, I'll try, to at least to some extent, fulfill my social task as a scientist who has been involved in this field for a long time and intensively so, and to share some of my thoughts with everyone who has started to feel anxious about this new pandemic in the 21st century.
In addition, I have agreed to be a guest of Mr. Aleksander Stankovic this Sunday, 03/01/2020. on the "Sunday at 2" show. On top of that, I also agreed to accept an interview from Nenad Jaric Dauenhauer for Index.hr which should be published a week later, on around 08/03/2020.
As well as that, I'll write something for "Vecernji list", of which I'm a columnist. All other media have the right to publish sequels to the series I started on Facebook called "Quarantine Wuhan", in which, throughout the course of this pandemic, I'll systematically explain everything that I think is essential for in-depth understanding and good information about everything that's going on. I really won't be able to offer much more than that, so I'd like to sincerely apologise to everyone in advance.
Whenever I return to Croatia for shorter or longer visits, my friends humorously warn me: "Igor, here in Croatia, caution is not enough. Paranoia is needed!". If this is true, I'm afraid some people have begun to apply this kind of thinking to the new coronavirus situation. I'd like to say that caution is still sufficient in this case, but paranoia is not really needed.
But the question is just how much caution should this be? Although it's not right for a serious scientist to predict anything about the spread of a completely new and unknown virus to the entire human population in the world, and to predict each individual event, over the past two months, we've gathered enough information about the new COVID-19 coronavirus for at least some predictions.
If the new coronavirus completely spreads over Croatia over time and manages to circumvent the many preventive measures currently in place, its casualties should be at least approximately comparable to the deaths from flu or road traffic accidents over the same period. This means that some sound caution is advisable. This caution is reasonable as long as it's at the same level as the mild concern you may feel when sitting in your car preparing for a longer journey, or when you hear on the news that the flu has arrived in Croatia.
If you feel the fear of the new coronavirus more than when you sit behind the wheel or hear that the flu is already well known to you, it means that that fear is no longer reasonable and that you've begun to succumb to panic. This panic is triggered by the constant media coverage and the way it's highlighted, rather than by the generally accepted and scientifically based knowledge of coronavirus. If you've started to behave differently than you usually do during the winter months, during the flu epidemic, for example, such collecting food supplies or wearing masks down the street, this is again not a behaviour that is in line with the actual magnitude of the danger.
People these days, however, often ask me why is so much written about coronavirus and why do people care so much, when the same level of attention isn't given to flu, given that flu may be a more dangerous disease? The reason is partly because flu has been a well-known disease for decades, comes back every year, and we have experience with its manifestation in tens of millions of people worldwide, we know how to develop vaccines against it beforehand, and we've started to get the first somewhat effective drugs out onto the market.
Unlike the flu, the new coronavirus is unknown to us and we're most cautious about not being surprised by it. If this virus is of any interest at the moment, then it's to adapt to the human species as its new reservoir in which it will continue to multiply, and not kill us.
The virus, now spreading through the human species, continues to mutate in order to adapt to us as quickly as possible. Many of these mutations will make it less dangerous for our health, as it will make us more fit. However, some random mutations could make it more dangerous, and we need to be on our guard until we get better acquainted with it and the pandemic is over. It's unlikely that this new coronavirus will mutate in such a way that it could become significantly more dangerous in those who have been infected than it is now, but we'll definitely be able to assert that only when the pandemic is over.
I hope that these thoughts will at least calm my readers a little bit, and I'll offer more detailed information, if everything goes to plan, on the "Sunday at 2" programme, in my interview for Index.hr, in my new columns in ''Vecernji list'', and continuously here on Facebook, as well as through the "Quarantine Wuhan" series, which will slowly follow the development of this pandemic and its most interesting stories.
I'd also like to point out to Croatian media representatives that our top scientist Petra Klepac works at the famous London School of Hygiene and Tropical Medicine, and she is involved in the modelling of infectious diseases, namely possible epidemics and pandemics of coronaviruses. If you know of more Croatian experts in the world who are involved in this field, be sure to refer to them in the comments below. Also, help share this by making this expert view of the coronavirus go "viral" before the coronavirus itself in Croatia becomes "viral", so there will be less unnecessary fear.
Thank you all for your interest and feel free to share my follow-up posts on the pandemic.
Prof. dr. sc. Igor Rudan, FRSE
Director of the Center for Global Health, University of Edinburgh
Director of the World Health Organization Collaborative Center, University of Edinburgh
Editor-in-Chief of the International Journal of Global Health''
This text was written by Igor Rudan and translated by Lauren Simmonds
For rolling information and updates in English on coronavirus in Croatia, as well as other lengthy articles written by Croatian epidemiologist Igor Rudan, follow our dedicated section.


